Pancreatic Function Test: Simple Explanation and What to Expect
If your doctor mentioned a pancreatic function test, you might wonder what that actually means. In plain terms, it’s a set of lab checks that tell you how well your pancreas is doing its two main jobs: releasing digestive enzymes and controlling blood sugar.
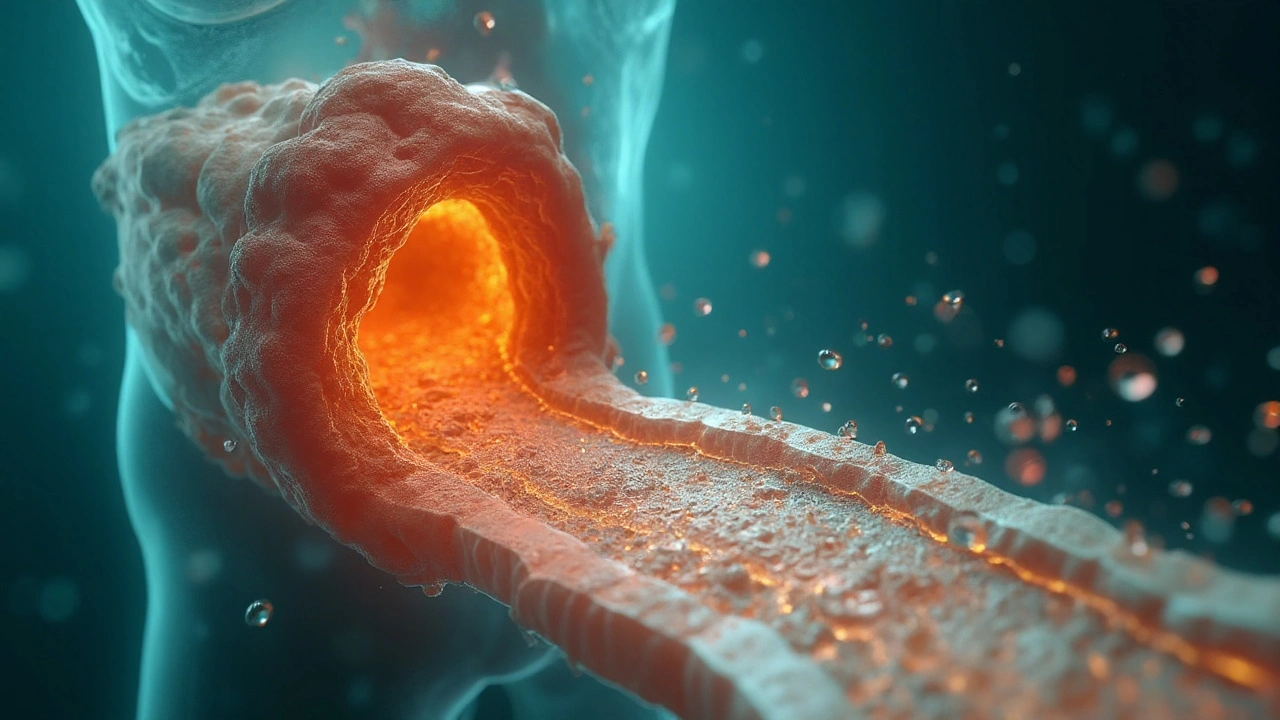
The pancreas produces enzymes like amylase and lipase that break down food in your gut. It also makes insulin, the hormone that moves glucose from your bloodstream into cells. When either of these roles goes off‑track, you can feel abdominal pain, get unexpected weight loss, or see odd blood‑sugar swings. That’s why a quick blood draw or a stool sample can give doctors a solid clue about what’s going on.
Why Doctors Order the Test
Doctors use pancreatic function tests for a few practical reasons. First, if you have persistent belly pain, nausea, or unexplained diarrhea, the test can help spot pancreatitis – inflammation that shows up as high amylase or lipase levels. Second, if you’re being evaluated for diabetes or unexplained low blood sugar, the test may include a fasting glucose or a short‑term glucose tolerance check to see how well your pancreas makes insulin.
Another common scenario is monitoring chronic conditions like cystic fibrosis or long‑term alcohol use. In those cases, a fecal elastase test (a stool sample) shows whether the pancreas is still delivering enough enzymes to the intestine. Low elastase means you might need enzyme supplements to keep digestion smooth.
Understanding Your Results
When the lab returns, you’ll usually see numbers for amylase, lipase, and perhaps fecal elastase. Normal amylase is roughly 30‑110 U/L, while lipase sits around 0‑160 U/L, but each lab sets its own range. A spike in either enzyme often points to acute pancreatitis, especially if you have recent heavy alcohol use, gallstones, or a high‑fat meal that triggered an attack.
If the enzyme levels are low, it might signal chronic pancreatitis or a blockage that’s preventing enzyme release. In that situation, doctors may suggest a pancreatic enzyme replacement therapy (PERT) to improve nutrient absorption.
For the glucose side, a fasting blood sugar under 100 mg/dL is considered normal. If your doctor runs a 2‑hour oral glucose tolerance test, numbers below 140 mg/dL after the drink are typically fine. Higher readings can mean impaired glucose tolerance or early‑stage diabetes, prompting lifestyle tweaks or medication.
It’s easy to get nervous looking at numbers you don’t understand. The key is to remember that the test is a snapshot, not a verdict. Your doctor will combine these results with your symptoms, medical history, and sometimes imaging (like an abdominal ultrasound) to form a full picture.
So, what should you do next? If any values are out of range, ask your doctor what the next steps are. Might you need a repeat test, a referral to a gastroenterologist, or an enzyme supplement? If everything looks normal but you still feel off, discuss other possibilities – sometimes the issue lies elsewhere, like with the gallbladder or small intestine.
Bottom line: a pancreatic function test is a quick, low‑risk way to check two critical jobs that your pancreas does every day. Understanding the why, what, and how turns a mysterious lab order into a useful tool for keeping your digestion and blood‑sugar levels on track.
Secretin Explained: Science, Safety, and Real-World Uses of the Secretin Supplement
What secretin is, what the science says, who it helps, and why most "secretin supplements" won’t work. Evidence, safety, and practical next steps in 2025.