
Every time you pick up a new prescription, you get a small paper booklet-the Medication Guide. It’s not just filler. This is your lifeline to understanding the real risks of your medicine. The FDA requires these guides for drugs with serious, preventable dangers. If you skip reading it, you’re flying blind. You might miss that your medicine could damage your liver, lower your white blood cells, or trigger dangerous mood changes. And worse-you might not know when to call your doctor or when to rush to the hospital.
What Makes a Medication Guide Different
Not all drug information is the same. The package insert your doctor gets is full of technical jargon. The Medication Guide is different. It’s written for you. By law, it must use plain language-at a 6th to 8th grade reading level. It can’t say "may cause adverse reactions." It has to say something like, "This medicine can cause serious liver damage." No fluff. No hiding behind vague words. There are about 150 of these guides in the U.S. right now. They cover everything from antidepressants to blood thinners to cancer drugs. The FDA updates them constantly. If a new safety issue pops up, the manufacturer has just 30 days to fix the guide. In 2022, 92% of them got updated. That means even if you read one last year, it might be outdated now. And here’s the kicker: pharmacies are supposed to give you one every time you fill the prescription. But a 2022 audit found that 41% of independent pharmacies didn’t always do it. If you don’t get one, ask for it. Don’t leave without it.The Seven Sections You Must Know
Every Medication Guide follows the same structure. You don’t need to read every word, but you must find these seven sections:- What is the most important information I should know? This is where the FDA puts the biggest warnings. Look for phrases like "can cause," "may lead to," or "serious risk." This is your red flag zone.
- What should I tell my healthcare provider before taking this medicine? This tells you who shouldn’t take it. If you have liver disease, kidney problems, or a history of depression, this section tells you if it’s safe for you.
- What are the possible or reasonably likely serious side effects? This is where the monitoring instructions live. This is the section that saves lives.
- How should I take this medicine? It tells you dosage, timing, and-critically-when to get blood tests or check-ins.
- What should I avoid while taking this medicine? Alcohol? Sunlight? Driving? This tells you what to skip.
- What are the possible common side effects? These are things like headache or nausea. Not dangerous, but annoying.
- How should I store this medicine? Simple, but important. Some drugs need refrigeration. Others must stay dry.
Where the Real Safety Info Hides
The most important part isn’t the first page. It’s the section that says: "What are the possible or reasonably likely serious side effects?" This is where the monitoring rules live. Take warfarin (Coumadin). The guide says: "Your healthcare provider should check your INR at least once a month. If your dose changes, check it more often." It doesn’t say "maybe check your blood." It says exactly how often. And it lists symptoms that mean trouble: unusual bruising, bleeding that won’t stop, coughing up blood. Clozapine (Clozaril) says: "About 1 in 200 people taking this medicine may develop agranulocytosis." That’s a life-threatening drop in white blood cells. So it requires weekly blood tests for the first six months. No exceptions. Antidepressants? They all say the same thing: "Pay close attention to any changes, especially sudden changes, in mood, behavior, thoughts, or feelings. This is very important when the medicine is started or when the dose is changed." That’s not a suggestion. It’s a warning that suicide risk can spike in the first 4-6 weeks. These aren’t guesses. They’re based on real data. The FDA found that patients who followed the monitoring instructions had 32% fewer serious side effects.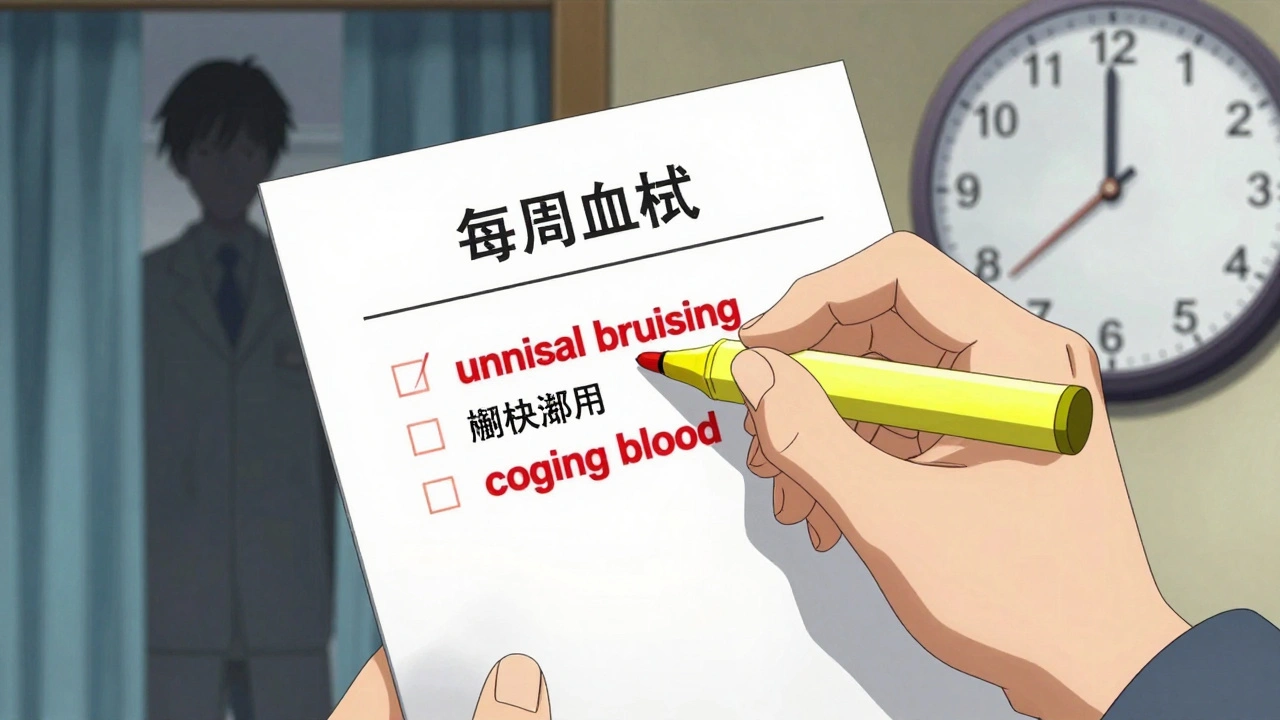
How to Read It Like a Pro
You don’t need to be a doctor. You just need a system. Step 1: Find the "Most Important Information" section. Read it first. If it says "can cause liver failure," you need to know what that means. Ask your pharmacist: "What are the signs of liver damage?" Step 2: Highlight every word that says "test," "monitor," "check," or "measure." Use a yellow marker. Circle the time frames: weekly, monthly, before starting, after 3 months. Underline symptoms that need emergency care in red. Step 3: Match the monitoring to the "How to Take" section. If the guide says, "Get blood tests every 3 months," but the "How to Take" section says, "Your doctor will schedule tests at your first visit and then every 6 weeks," which one is right? Call your doctor. There might be a conflict, or your doctor might have a different plan. Step 4: Use the "traffic light" system. Green = normal side effect (mild headache). Yellow = watch for this (dizziness that lasts more than a day). Red = go to the ER (chest pain, trouble breathing, black stool). Write this on a sticky note and put it on your medicine bottle. Step 5: Keep a medication journal. Write down your test dates. Did you get your blood drawn? Did your INR go up? Did you feel more anxious after the dose change? This helps your doctor spot patterns. A 2022 University of Michigan study found patients who did this had 68% fewer bad reactions.What to Do When It’s Confusing
Let’s be honest-some guides are still hard to read. Cancer drug guides, for example, get the lowest patient ratings. Why? They’re full of scary terms like "myelosuppression" and "cytokine release syndrome." Here’s what to do:- Go to DailyMed (dailymed.nlm.nih.gov). It’s the NIH’s official site. Search your drug name. You’ll get the latest guide in plain text.
- Watch for QR codes on the packaging. Newer drugs now have them. Scan it and you’ll go straight to the current guide.
- Ask your pharmacist to walk you through it. One pharmacist in New Zealand found that when she spent just 90 seconds pointing out the monitoring section, patient compliance jumped from 45% to 82%.
- Don’t trust your memory. Write it down. Take a photo of the key section with your phone.

Why This Matters More Than You Think
Medication Guides aren’t just paperwork. They’re a safety net. And that net is getting stronger. Starting in 2025, Medicare will penalize pharmacies that don’t hand out guides. That means you’ll get them more consistently. The FDA is also testing AI tools that personalize guides based on your age, health history, and other meds. Pfizer’s pilot showed patients understood risks 63% better when the guide focused only on what applied to them. But here’s the hard truth: 40% of Americans still struggle to understand basic health info. That’s why the FDA’s next big move is pictograms-simple icons that show when to test, when to call, when to stop. By 2026, you’ll see these on every guide. Right now, you have the power to protect yourself. You don’t need to memorize every detail. Just learn to find the three things: what’s dangerous, when to test, and when to call for help.Common Mistakes People Make
A 2022 survey found 63% of patients misunderstood monitoring instructions. Here’s what goes wrong:- "Monitor monthly" means "get a blood test once a month," not "pay attention if you feel weird."
- "Call your doctor immediately if..." means right now-not tomorrow, not next week.
- "Don’t stop without talking to your doctor" means don’t quit because you feel better. Stopping suddenly can cause seizures or heart problems.
- "Avoid sunlight" doesn’t mean "don’t go outside." It means wear sunscreen, cover up, and avoid tanning beds.
What to Do Next
Today, when you pick up your next prescription:- Ask for the Medication Guide.
- Find the "Most Important Information" section.
- Circle the time-based monitoring instructions.
- Underline the emergency symptoms.
- Write down the next test date on your calendar.
Do I need to read the Medication Guide every time I refill my prescription?
Yes. Even if you’ve taken the medicine before, the guide can change. New safety warnings, updated monitoring schedules, or new drug interactions can appear. The FDA requires manufacturers to update guides within 30 days of new risk data. Always check the date on the guide. If it’s older than your last refill, ask your pharmacist for the latest version.
What if my pharmacy doesn’t give me a Medication Guide?
Ask for it. By law, pharmacies must provide a Medication Guide every time a drug with one is dispensed. If they say they don’t have it, call the manufacturer’s patient help line-the contact info is usually on the drug’s website. You can also download the current guide from DailyMed (dailymed.nlm.nih.gov). Never leave without it.
Can I rely on my doctor to explain all the risks?
Your doctor should explain major risks, but they’re often pressed for time. Medication Guides are designed to fill the gaps. They’re written by experts and reviewed by the FDA to ensure nothing critical is missed. Think of the guide as your second opinion. Use it to ask better questions during your visit.
Are Medication Guides the same as the patient leaflets I get in other countries?
No. U.S. Medication Guides are more detailed on monitoring and risk, especially for serious side effects. European patient leaflets often include more visuals and use simpler language, but they don’t always specify how often to get blood tests or what exact symptoms require emergency care. If you’re traveling or using a drug made abroad, always check the U.S. version on DailyMed for the most complete safety info.
How do I know if the Medication Guide I have is the latest version?
Look at the date on the first page. Then go to DailyMed (dailymed.nlm.nih.gov), search your drug name, and compare the dates. If your paper guide is older than the one online, you have an outdated version. Ask your pharmacist for the current one. Some newer packages have QR codes that link directly to the latest guide-scan it to be sure.
Write a comment
Your email address will not be published.



8 Comments
bro i just scanned the QR code on my antidepressant bottle and it showed me i need monthly INR checks?? i’ve been taking this for 2 years and never knew. my doctor never mentioned it. now i’m scared to even sleep. 😵💫💊
Of course. The FDA. The same agency that approved Vioxx, then acted shocked when people started dropping dead. And now they want us to trust a 6th-grade pamphlet? Please. The real danger is that these guides are written by lawyers, not doctors. And if you think your pharmacist gives a damn? Ha. They’re paid by the pill, not by your survival.
Ask for the guide. Highlight the red flags. Write down your test dates. That’s it. Five minutes. Could save your life.
This is actually really helpful. I’m from Nigeria and we don’t get these guides here. My cousin died last year from a reaction to a blood pressure med-no one told him to check his potassium. I’m printing this out and sharing it with my family. Thank you.
While the intent of the Medication Guide is laudable, its efficacy remains severely compromised by the structural inadequacies of the American pharmaceutical education infrastructure. One cannot reasonably expect the layperson to interpret clinical risk stratification without prior exposure to biomedical literacy frameworks. This is not a solution-it is a performative gesture of regulatory compliance masquerading as patient empowerment.
so i just found out my anxiety med says 'watch for sudden mood swings'... wait. that’s me. every time i get mad at my cat. 🤔
They’re updating these guides every 30 days? That’s not safety-it’s manipulation. They’re changing the language to scare people into staying on the drug. Did you know the FDA gets funding from Big Pharma? They’re not protecting you. They’re protecting profits. And now they’re adding QR codes? That’s how they track you. Don’t scan anything.
Thank you for this. I’ve been teaching this to my patients for years, but most never listen. I’m going to print this and hand it out. One thing I’d add: if the guide says 'call immediately' and you’re not sure-call anyway. Better to be the person who cried wolf than the one who didn’t call until it was too late. We’re all just trying to stay alive here.