
Drowsiness Duration Calculator
Your Drowsiness Duration Estimate
Based on your inputs
This is an estimate based on clinical studies showing typical drowsiness duration after first-generation antihistamines like diphenhydramine (Benadryl)
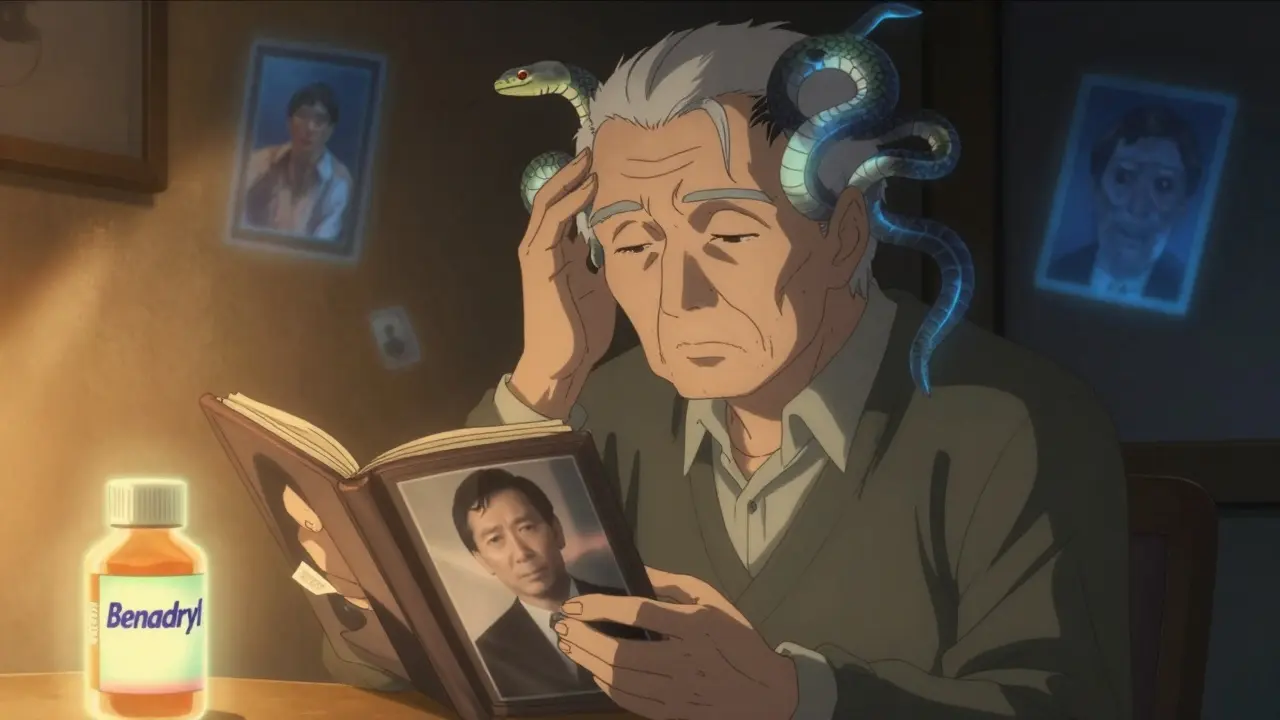
Most people reach for Benadryl when they get hives or a stuffy nose. It’s cheap, easy to find, and works fast. But what happens when that quick fix leaves you feeling like you’ve been knocked out for hours - or worse, makes it hard to remember your own name the next morning? First-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine don’t just block allergies. They also slam into your brain and mess with your body’s natural chemistry in ways most labels don’t warn you about.
How These Drugs Actually Work (And Why They Hit Your Brain)
First-generation antihistamines were designed to stop histamine from triggering allergy symptoms. But unlike newer versions, they’re small, oily molecules that slip right through the blood-brain barrier. Once inside, they don’t just block histamine receptors - they bind to muscarinic receptors too. That’s the same system that controls saliva, bladder control, pupil size, and memory.
Think of it like a key that fits two locks. One lock is the histamine receptor (good for allergies). The other is the muscarinic receptor (bad for your brain and body). That’s why you get dry mouth, blurry vision, trouble peeing, and that heavy, foggy feeling. Studies show these drugs can occupy 30-50% of brain H1 receptors at standard doses. Compare that to second-generation antihistamines like loratadine or cetirizine - they barely touch the brain, staying under 5% receptor occupancy.
It’s not magic. It’s chemistry. Diphenhydramine reaches brain concentrations of 15-25 ng/mL within two hours. That’s enough to slow reaction times like alcohol. In driving simulators, users perform as badly as people with a 0.05% blood alcohol level. And that impairment doesn’t vanish after 6 hours. For some, it lingers for up to 18 hours.
The Real Cost of That “Sleepy” Feeling
People often say, “I just take it at night to sleep.” And sure, it works - for a while. But that sleep isn’t restorative. It’s sedation. And the next-day hangover? It’s real. A 2022 survey of over 1,200 older adults using low-dose diphenhydramine for sleep found 42% reported morning confusion lasting 3-4 hours. That’s not just groggy. That’s impaired judgment, slower reflexes, and higher fall risk.
And it’s not just seniors. Young people are getting caught too. Reddit users report waking up at 2 p.m. after taking Benadryl at 8 p.m. - feeling like they’d been hit by a truck. One user wrote: “Took it for mild hives. Woke up groggy, forgot my kid’s name for 10 minutes. Not worth it.”
Even if you don’t feel sleepy, your brain is still affected. Studies show a 20-30% drop in attention and reaction time - even when users think they’re fine. That’s why emergency rooms see so many cases of drowsy driving linked to these drugs. In 2021, 35% of drowsy driving crashes involved first-gen antihistamines, according to NHTSA data.
Anticholinergic Effects: More Than Just Dry Mouth
Dry mouth? That’s the least of it. Anticholinergic effects mean your body’s “rest and digest” system is being shut down. Your pupils dilate. Your bladder won’t empty. Your stomach slows down. Your heart races. For younger people, this might just mean discomfort. For older adults, it’s dangerous.
The American Geriatrics Society calls first-generation antihistamines “potentially inappropriate” for people over 65. Why? Because long-term use increases dementia risk by 54%. That’s not a small bump. That’s a clear, proven link. Every pill adds up. Cumulative anticholinergic burden - the total amount of these drugs your body has processed over months or years - is now recognized as a major risk factor for cognitive decline.
And it’s not just memory. Urinary retention is common. One WebMD forum user said, “I started taking Benadryl for allergies and ended up needing a catheter.” That’s not rare. About 28% of long-term users report urinary issues consistent with anticholinergic effects.
When They Might Still Make Sense
That doesn’t mean these drugs have no place. They’re still the most effective option for motion sickness - 70-80% success rate, compared to 40-50% for second-gen drugs. They’re also the fastest-acting for acute allergic reactions. If you’re having a sudden, severe reaction and need relief within 15 minutes, diphenhydramine still wins.
They’re also the go-to for short-term insomnia. For someone who can’t sleep for one night and has no other options, a low dose (12.5-25 mg) can help. But it’s not a long-term solution. The brain adapts. Tolerance builds. And the side effects pile up.
The American College of Allergy, Asthma, and Immunology says these drugs should only be used for short-term, specific needs - not daily allergy control or routine sleep aid.
Why OTC Labels Don’t Tell the Whole Story
Look at the bottle. “May cause drowsiness.” That’s it? No mention of next-day fog. No warning about dementia risk. No note that it can make you fail a breathalyzer test. A 2022 JAMA study found 45% of users underestimate how long the impairment lasts. Most think it’s gone in 6-8 hours. Reality? Up to 18.
Pharmaceutical companies know this. That’s why the FDA pushed for stronger labeling in 2022. But OTC packaging hasn’t caught up. You’ll find bigger warnings on prescription promethazine than on a $5 bottle of generic Benadryl.

What to Do Instead
If you’re using first-gen antihistamines for allergies or sleep, ask yourself: Is this the best option? For daily allergy control, second-generation drugs like loratadine, cetirizine, or fexofenadine are safer. They work just as well - without the brain fog. They cost more, sure. But a $15 bottle lasts 30 days. A $5 bottle of diphenhydramine might cost less, but it’s costing you your focus, your safety, and maybe your long-term brain health.
For sleep? Try melatonin, good sleep hygiene, or cognitive behavioral therapy for insomnia (CBT-I). They’re more effective long-term and don’t mess with your nervous system.
If you’re using these drugs for motion sickness or nausea, talk to your doctor. There are alternatives like scopolamine patches that don’t cause the same level of cognitive impairment.
Red Flags You’re Taking Too Much
- You feel foggy or sluggish even 12 hours after taking it
- You’ve had trouble urinating or feel like your bladder won’t empty
- You’re forgetting names, dates, or where you put things
- You’re using it more than 2-3 times a week
- You’ve started taking it without a clear reason - just “to help me relax”
If any of these sound familiar, it’s time to reconsider. Talk to your doctor. Switch to a second-gen antihistamine. Or better yet - stop using them altogether if you don’t need them.
What’s Next for These Drugs?
Pharma companies are already working on “third-generation” antihistamines designed to avoid the brain entirely. Two candidates, EB-029 and DP-118, are in Phase II trials and show 80% less brain penetration - while keeping the allergy-fighting power. The FDA is also reviewing restrictions on pediatric use after a 27% spike in ER visits from misuse between 2018 and 2022.
Market analysts predict first-gen antihistamine sales will drop 15-20% by 2030 as cheaper, safer alternatives become more common. But until then, millions keep buying them - unaware of what they’re really doing to their brains.
You don’t need to be a scientist to understand this: if a drug makes you drowsy, foggy, or unable to focus, it’s not helping you - it’s masking your symptoms with side effects that could hurt you long-term.
Are first-generation antihistamines safe for seniors?
No. The American Geriatrics Society specifically lists them as potentially inappropriate for people over 65. They increase the risk of falls, confusion, urinary retention, and dementia. Studies show chronic use raises dementia risk by 54%. Even low doses taken over months can add up. Safer alternatives like second-generation antihistamines or non-drug treatments should be used instead.
How long does drowsiness from Benadryl last?
Most people think it wears off in 6-8 hours. But studies show cognitive impairment can last up to 18 hours after a single dose. Driving simulators and reaction tests confirm this. Even if you feel fine, your brain is still slowed. That’s why many people don’t realize they’re impaired until they’re behind the wheel or operating machinery.
Can I take first-gen antihistamines with alcohol?
Never. Alcohol increases brain penetration of these drugs by 40-60%. It multiplies sedation, impairs coordination even more, and raises the risk of overdose. Mixing them is like doubling your dose without realizing it. Emergency rooms see this combo often - and it’s deadly.
What are the best alternatives to Benadryl for allergies?
Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are second-generation antihistamines. They work just as well for allergies but don’t cross into the brain. You won’t feel drowsy. No brain fog. No next-day hangover. They cost a bit more, but they’re far safer for daily use - especially if you drive, work, or care for kids.
Is it okay to use diphenhydramine every night to sleep?
No. While it helps you fall asleep, it doesn’t improve sleep quality. It suppresses REM sleep and causes next-day grogginess. Long-term use is linked to cognitive decline. Better options include melatonin, sleep hygiene, or CBT-I - all proven to help without the risks. Don’t treat insomnia with a drug that harms your brain.
Do these drugs interact with other medications?
Yes. First-gen antihistamines are metabolized by liver enzymes CYP2D6 and CYP3A4. That means they can interact with antidepressants, heart medications, painkillers, and even some antibiotics. People who are poor metabolizers of CYP2D6 can have 2-3 times higher drug levels in their brain - leading to extreme drowsiness or toxicity. Always check with your pharmacist before combining them with other meds.
If you’re using a first-generation antihistamine right now, ask yourself: Am I using it because it’s the best choice - or just because it’s the easiest one to grab off the shelf? The answer might change everything.
Write a comment
Your email address will not be published.



13 Comments
Let’s be real - if you’re still taking Benadryl like it’s candy, you’re not managing your allergies, you’re just self-sabotaging. The data doesn’t lie: 54% higher dementia risk? That’s not a side effect, that’s a sentence. And no, ‘I only take it at night’ doesn’t make it okay. Your brain doesn’t care when you took it - it remembers every dose.
Benadryl = brain rot. Done.
The scientific rigor of this post is commendable. However, the casual tone and lack of formal citation of primary literature undermines its credibility. Peer-reviewed studies from the Journal of the American Geriatrics Society and the New England Journal of Medicine must be referenced to validate claims regarding anticholinergic burden and dementia risk. Without proper sourcing, this remains anecdotal.
I cried reading this. 🥺 I took Benadryl for years thinking it was ‘just helping me sleep’ - then I realized I was forgetting where I parked my car, forgetting my mom’s birthday, and almost crashed my bike because I couldn’t focus. I switched to Zyrtec. My brain came back. Thank you for writing this. Someone needed to say it.
Look, the entire OTC pharmaceutical industrial complex is predicated on the illusion of safety. First-gen antihistamines are the perfect example: low cost, high margin, zero accountability. The FDA’s toothless labeling requirements are a corporate giveaway. This isn’t negligence - it’s calculated exploitation. You think you’re saving money? You’re paying in cognitive decay. And the worst part? You’re complicit because you didn’t read the fine print. Wake up.
im so glad someone finally said this. i used to take benadryl every night for like 3 years and i just thought i was tired. turns out i was basically drunk all day. switched to claritin and now i can actually remember what i ate for lunch. thanks for this
There’s a deeper philosophical question here: when does convenience become a form of self-harm? We’ve normalized pharmacological sedation as a solution to modern life’s discomforts - sleeplessness, allergies, anxiety - but at what cost to our agency? The body remembers what the mind forgets. These drugs don’t cure; they suppress. And suppression, over time, becomes a slow erasure of the self.
This is a public health crisis disguised as a sleep aid. Stop normalizing brain fog. Your life is not a commodity to be traded for convenience. Act now.
Big shoutout to the OP - this is the kind of info we need more of. I used to give my kid Benadryl for car rides (thought it was harmless) until I read about the ER spikes in kids. Now I use the scopolamine patch. No more zombie mode. 🙌
People who take these drugs are just lazy. If you can’t handle a little drowsiness, maybe you shouldn’t be driving or working. This isn’t a crisis - it’s personal responsibility. Stop blaming the medicine and start blaming yourself for being weak.
The anticholinergic burden is the silent epidemic of our pharmacological age - a slow-motion neurodegenerative cascade disguised as relief. We’ve weaponized sedation as a lifestyle tool, and now the CNS is paying the piper. The third-gen candidates? They’re not just better - they’re a moral imperative.
If you're reading this and you're still using diphenhydramine daily - take a breath. You're not alone. I was there too. I switched to cetirizine. No more 3 p.m. crashes. No more forgetting my wife's name. I'm not saying it's easy - but it's worth it. You got this. 💪
How ironic that we’ve elevated the pharmacological suppression of natural biological signals - sleep, histamine response, cognitive clarity - to the status of wellness. This isn’t medicine. It’s spiritual anesthesia. The real tragedy isn’t the dementia risk - it’s that we’ve forgotten what it feels like to be awake.