One in two adults over 60 has a thyroid nodule-most don’t even know it. These small lumps in the thyroid gland are so common that doctors often find them by accident during routine ultrasounds or neck exams. But when you hear the word thyroid nodule, fear kicks in. Is it cancer? Do I need surgery? Do I even need a biopsy? The truth is, more than 90% of thyroid nodules are harmless. The real challenge isn’t finding them-it’s figuring out which ones actually need action.
What Makes a Thyroid Nodule Suspicious?
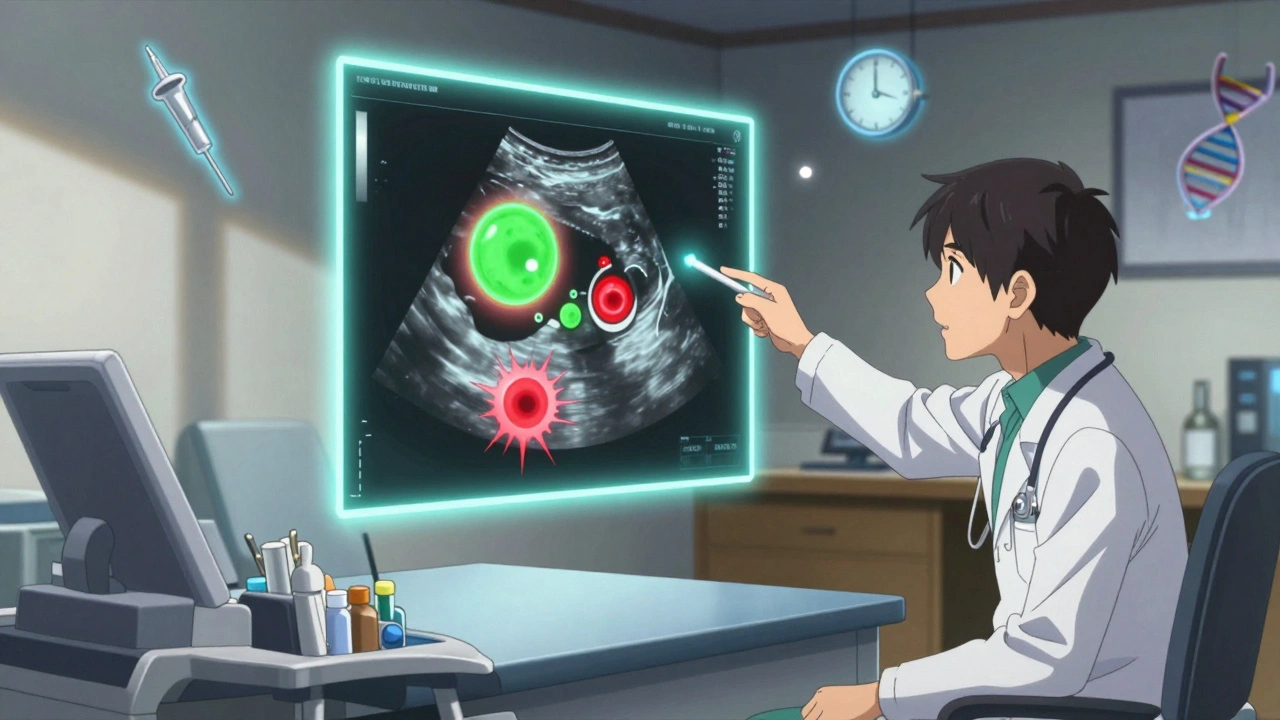
Not all nodules are created equal. The difference between a harmless bump and something dangerous comes down to size, shape, and how it grows. Ultrasound is the first tool doctors use to look at these nodules. It’s quick, painless, and shows details your fingers can’t feel. Malignant nodules often show specific signs: tiny calcium spots called microcalcifications, irregular or spiky edges, and a darker gray appearance (hypoechogenicity). These features raise red flags. Benign nodules, on the other hand, tend to be fluid-filled cysts, have smooth borders, or look spongy-like a honeycomb under the ultrasound. A 2017 study in the Journal of Clinical Endocrinology & Metabolism found that nodules with these suspicious features had up to 83% higher chance of being cancerous. Size matters too. The American Thyroid Association says any nodule over 1 cm should be checked. But here’s the catch: a 2 cm nodule that looks perfectly normal might be less worrisome than a 9 mm nodule with microcalcifications. That’s why doctors don’t just look at size-they look at the whole picture.How Fast Do Cancerous Nodules Grow?
Growth rate is one of the most reliable clues. A benign nodule might grow slowly-about 1 mm per year. A cancerous one? It often grows faster than 2 mm per year. That’s not much in absolute terms, but over time, it adds up. A 2017 study tracked over 1,000 nodules for five years. Those that grew more than 2 mm per year in at least two directions had more than three times the risk of being cancerous. That’s why doctors don’t just do one ultrasound and call it done. They schedule follow-ups-usually every 6 to 12 months-to measure changes. If a nodule jumps from 1.2 cm to 1.6 cm in a year, that’s a signal to act. Many people assume bigger = worse. But a 3 cm benign nodule might cause swallowing trouble or a lump in your throat, while a 7 mm cancerous one could be silent. That’s why growth speed matters more than size alone.When Is a Biopsy Actually Necessary?
Fine-needle aspiration (FNA) biopsy is the gold standard. It’s not surgery. It’s a thin needle, guided by ultrasound, pulling out a few cells. Results come back in about a week. The American Thyroid Association gives clear guidelines:- Biopsy if the nodule is ≥1 cm AND has suspicious ultrasound features
- Biopsy if it’s ≥1.5 cm with no suspicious features
- Biopsy if it’s ≥2 cm, no matter what it looks like
Benign vs. Cancerous: What’s Actually Inside?
Most benign nodules are either colloid nodules (just packed thyroid tissue) or follicular adenomas (non-cancerous tumors). Pure cysts-filled with fluid-are almost always harmless. Cancerous nodules? Over 80% are papillary thyroid cancer. It grows slowly, often spreads to neck lymph nodes, but has a 98% survival rate after treatment. Follicular cancer (10-15%) is trickier-it rarely spreads to lymph nodes but can travel through blood to lungs or bones. Medullary and anaplastic cancers are rare but aggressive. The key point: even if it’s cancer, it doesn’t mean you’re facing a life-threatening illness. Most thyroid cancers are highly treatable. The goal isn’t to remove every nodule-it’s to catch the dangerous ones early and leave the rest alone.Why So Many Unnecessary Biopsies Happen
Here’s the uncomfortable truth: too many people get biopsied for nodules that never needed it. In the 1990s, doctors biopsied almost every nodule over 1 cm. That led to tens of thousands of surgeries for cancers that would’ve never caused harm. Dr. Gilbert Welch from Dartmouth calls this “overdiagnosis.” He points out that thyroid cancer rates have jumped 15 times since 1975-not because we’re getting sicker, but because we’re scanning more. Many of these tiny cancers are found by accident and would never grow or spread. The result? One in three biopsies for indeterminate nodules turns out to be a false alarm. That means people underwent surgery for nothing-losing part of their thyroid, needing lifelong medication, and dealing with recovery. That’s why modern guidelines stress caution. Molecular testing now helps avoid 35% of unnecessary surgeries. And active surveillance-watching small, low-risk cancers without cutting-is becoming standard. A 2021 JAMA Surgery study showed 87% of microcarcinomas under 1 cm stayed stable over five years.What Happens After the Biopsy?
Results are grouped under the Bethesda System:- Category 1: Nondiagnostic (1-4% cancer risk) → repeat biopsy
- Category 2: Benign (0-3% risk) → monitor with ultrasound every 1-2 years
- Category 3: Atypia of undetermined significance (5-15% risk) → molecular test or repeat biopsy
- Category 4: Follicular neoplasm (15-30% risk) → surgery often recommended
- Category 5: Suspicious for malignancy (60-75% risk) → surgery
- Category 6: Malignant (97-99% risk) → surgery

What You Can Do Now
If you’ve been told you have a thyroid nodule:- Ask for the ultrasound report-get the exact size and features
- Find out if it’s growing-request a comparison to past scans
- Ask if molecular testing is an option, especially if biopsy was indeterminate
- Don’t panic over size alone-look at the whole picture
- Seek a second opinion if surgery is recommended without clear signs of cancer
What’s New in 2025?
New tools are making monitoring smarter. AI-powered ultrasound systems, like the FDA-cleared ThyroidAI, now analyze images with 89% accuracy-helping doctors spot subtle patterns humans might miss. Radiofrequency ablation is also gaining ground for large benign nodules that cause discomfort. It shrinks them without cutting, with fewer side effects than surgery. By 2025, nearly two-thirds of indeterminate nodules will be evaluated with molecular testing, cutting unnecessary surgeries by 25,000 per year in the U.S. alone. The goal isn’t to catch every tiny cancer-it’s to catch the ones that matter.Are all thyroid nodules cancerous?
No. Over 90% of thyroid nodules are benign. Most people with nodules never develop symptoms or need treatment. Cancer is rare, and even when it occurs, it’s often slow-growing and highly treatable.
Can a benign nodule turn cancerous?
It’s extremely rare. Benign nodules like follicular adenomas or colloid nodules don’t transform into cancer. But a new cancer can develop next to or within an existing benign nodule-this is why monitoring growth and ultrasound features matters more than assuming a nodule is permanently safe.
Do I need a biopsy if my nodule is under 1 cm?
Not automatically. If it’s under 1 cm and has no suspicious ultrasound features, most doctors will just monitor it. But if you have a history of radiation, family cancer, or rapid growth-even a small nodule may need a biopsy. Size isn’t the only factor.
What if my biopsy result is indeterminate?
Don’t panic. An indeterminate result means the cells look unusual but aren’t clearly cancerous. Ask your doctor about molecular testing (like ThyroSeq or Afirma). These tests can rule out cancer with over 95% accuracy in many cases, helping you avoid unnecessary surgery.
Can I just watch the nodule instead of biopsying it?
Yes-if it’s small, stable, and has no suspicious features. Active surveillance is now a standard option for low-risk nodules and even small papillary cancers. You’ll get ultrasounds every 6-12 months. If it stays the same, no action is needed. If it grows or changes, then you reassess.
Is thyroid cancer deadly?
For the vast majority, no. Papillary thyroid cancer-the most common type-has a 98% 10-year survival rate. Even when it spreads to lymph nodes, it responds well to surgery and radioactive iodine. Death from thyroid cancer is rare and usually linked to delayed diagnosis or rare, aggressive types like anaplastic cancer.
What’s the risk of a false positive biopsy?
About 30% of biopsies for indeterminate nodules (Category 3 and 4) turn out to be benign after surgery. That’s why molecular testing is now recommended-it reduces unnecessary surgeries by up to 35%. Always ask if molecular testing is available before agreeing to surgery.
What Comes Next?
If you’ve been told you have a thyroid nodule, your next step isn’t surgery. It’s understanding. Ask for your ultrasound report. Track growth over time. Push for molecular testing if your biopsy is unclear. Avoid rushing into surgery unless the evidence clearly points to cancer. Thyroid nodules are common. Cancer is not. The goal isn’t to remove every lump-it’s to find the few that truly need attention. With today’s tools, you don’t have to guess. You can know.Write a comment
Your email address will not be published.




8 Comments
Had a 1.4cm nodule last year-no microcalcifications, smooth edges. Doctor wanted to biopsy immediately. I pushed back, asked for a repeat ultrasound in 6 months. It didn’t budge. Turned out to be a colloid nodule. Sometimes the system rushes to cut before it even understands what it’s looking at. I’m alive, thyroid intact, and I didn’t even need coffee for a week after the scan. 🤷♀️
So let me get this straight-we’re spending billions scanning every neck in America just to find cancers that won’t kill anyone, then cutting out glands so people need synthetic thyroid for life? Classic healthcare theater. Next they’ll biopsy freckles because ‘they might turn into melanoma.’ At this point, I’m just waiting for the ad: ‘Thyroid Nodule? Get your 30% off biopsy coupon today!’
OMG I just found out I have a nodule and I was like OH NOOO but then I read this and now I’m like… maybe it’s chill?? I’m gonna ask for the ultrasound report and not panic!! Thank you for writing this like a real human and not a robot doctor 😭💖
The real issue isn’t whether nodules are dangerous-it’s whether our medical infrastructure can handle uncertainty. We’re trained to fix, not to wait. To act, not to observe. But biology doesn’t care about our need for closure. A nodule that grows 1.8mm/year isn’t a ticking bomb-it’s a quiet anomaly. The courage isn’t in removing it. It’s in leaving it alone and trusting time.
lol they said 90% are benign but did you know the FDA and pharma companies are in cahoots? They want you to get biopsied so you buy levothyroxine for life. That’s why they invented ‘indeterminate’-so you panic and get surgery. Also, AI ultrasound? Nah. That’s just a fancy way to make you pay more. I’ve got a nodule and I’m just eating kelp and praying. It’s 2025, not 1985.
So what? You got a nodule. Big deal. Everyone’s got something wrong with them. You’re not special. You’re not going to die. You’re just gonna be on meds forever. Congrats. Now go get your biopsy so you can start your new life as a walking pharmacy.
THIS. This is the kind of info we NEED. 🙌 I’m so glad I didn’t rush into surgery after my nodule was found. I asked for molecular testing and it came back negative-no surgery, no meds, just peace. To anyone reading this: you’re not alone, you’re not doomed, and you deserve to make informed choices. 💪❤️
While your article is superficially well-structured, it fundamentally misunderstands the clinical epistemology of thyroid diagnostics. The Bethesda system, while widely adopted, lacks robust Bayesian calibration against population-level incidence curves. Furthermore, the reliance on ultrasound morphology as a surrogate for malignancy ignores the heterogeneity of follicular variant papillary carcinoma. Molecular testing, while promising, is still plagued by false negatives in RAS-mutated nodules. You’re not educating patients-you’re commodifying reassurance.