
When a senior falls, the fear isn’t just about a bruise or a sore hip. It’s about bleeding inside the brain - and for many older adults on blood thinners, that fear stops them from taking a medicine that could save their life. Anticoagulants reduce stroke risk by up to two-thirds in people with atrial fibrillation, yet nearly half of seniors over 85 aren’t taking them. Why? Because doctors and families worry that a fall could turn deadly. But the data tells a different story.
Stroke Risk Goes Up With Age - Fast
Atrial fibrillation, an irregular heartbeat, affects about 9% of people 65 and older. And the risk of stroke doesn’t creep up - it jumps. At 50-59, the chance of a stroke in a year is 1.5%. By 80-89, it’s 23.5%. That’s more than one in four. Without treatment, nearly one in five elderly patients with atrial fibrillation will have a stroke within a year. Most of those strokes are disabling or fatal.Anticoagulants Work - and They Work Better Than Aspirin
Warfarin, the old-school blood thinner, cuts stroke risk by about 64%. But newer drugs - dabigatran, rivaroxaban, apixaban, and edoxaban - do just as well, often better. Apixaban, for example, reduced stroke and clots by 21% compared to warfarin in people over 75. And here’s the kicker: they cause fewer dangerous brain bleeds. Rivaroxaban lowers intracranial hemorrhage risk by 34%. Dabigatran cuts stroke risk by 88% compared to placebo. Aspirin? It’s not enough. Studies show it only reduces stroke risk by 22%. That’s why guidelines stopped recommending it for stroke prevention in atrial fibrillation over a decade ago. Yet, many seniors still get it because it’s familiar. It’s not the right tool for this job.Fall Risk Doesn’t Mean Stop the Medicine
The biggest reason seniors don’t get anticoagulants? Fear of falls. And yes - if you’re on a blood thinner and fall, you’re more likely to bleed. In Minnesota hospitals, elderly patients on anticoagulants had a 50% higher chance of brain bleeding after a fall than those not on them. Ninety percent of fall-related deaths involved people over 85 or on blood thinners. But here’s what the studies don’t say: stroke kills more often than falls. A 2015 study of 24,000 patients over 75 found that the oldest patients - those 85 and up - got the greatest net benefit from anticoagulants. Why? Because their stroke risk was sky-high. Even with multiple falls, the math still worked: for every 100 octogenarians treated, 24 strokes were prevented versus 3 major bleeds. That’s 21 lives saved or spared from disability. The American College of Cardiology, American Heart Association, and Heart Rhythm Society all say age alone shouldn’t stop anticoagulation. And neither should a history of falls. The 2023 Journal of Hospital Medicine called discontinuing anticoagulants because of fall risk “inappropriate practice.”DOACs Are Safer - But They Have Limits
Direct oral anticoagulants (DOACs) are now the go-to for seniors. They don’t need regular blood tests like warfarin. Dosing is fixed. They’re easier to manage. But they’re not perfect. Most DOACs are cleared by the kidneys. As people age, kidney function drops. A 90-year-old might need a lower dose - or even avoid certain drugs. Dabigatran is 80% removed by the kidneys. Apixaban is 27%. If kidneys are weak, doctors adjust the dose or pick a safer option. Reversing bleeding used to be hard. Warfarin had vitamin K and fresh plasma. DOACs didn’t. Now, we have antidotes: idarucizumab for dabigatran, andexanet alfa for apixaban and rivaroxaban. These aren’t magic bullets, but they give doctors a tool - and that changes the game.It’s Not About the Drug - It’s About the Plan
Just giving a pill isn’t enough. The real work starts after the prescription is written. Seniors on anticoagulants need a full fall prevention plan:- Assess fall risk - Use tools like the Morse Fall Scale or a home safety check. Are there loose rugs? Poor lighting? No handrails?
- Review all meds - Benzodiazepines, sleep aids, opioids, even some blood pressure drugs can make you dizzy. Cut what you can.
- Move more - The Otago Exercise Program reduces falls by 35%. Simple balance and strength training - done at home - makes a huge difference.
- Monitor kidney function - Get a blood test every 6-12 months. Adjust dose if needed.
- Watch for signs of bleeding - Unexplained bruising, dark stools, headaches after a bump. Don’t wait.
Why So Many Seniors Are Still Left Untreated
Despite clear guidelines, only 48% of seniors over 85 get anticoagulants. In the 65-74 group, it’s 72%. That gap isn’t because the older patients are sicker - it’s because doctors are scared. A 2021 survey found 68% of primary care doctors would refuse anticoagulation for an 85-year-old who’d fallen twice in the past year - even if their stroke risk score was high. That’s not evidence-based. That’s fear. Patients and families often buy into it too. Reddit threads are full of caregivers saying, “My dad’s doctor won’t prescribe anything because he falls.” But the science says: untreated atrial fibrillation is far more dangerous than a fall.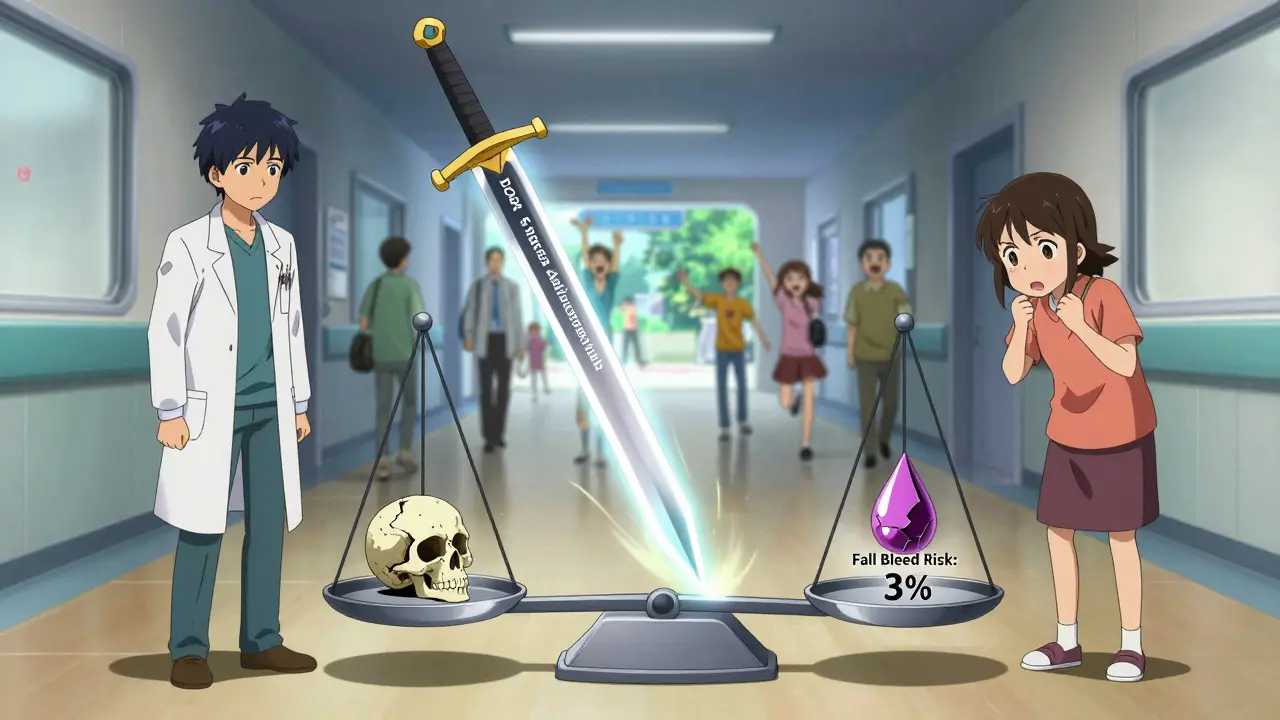
What You Should Do Right Now
If you or someone you care for is over 65 and has atrial fibrillation:- Ask for a CHA₂DS₂-VASc score. This calculates stroke risk. If it’s 2 or higher, anticoagulation is recommended.
- Ask if DOACs are an option. Apixaban is often best for seniors - it has the lowest bleeding risk in this group.
- Ask about kidney function. A simple creatinine test can guide dosing.
- Ask for a fall prevention plan. Don’t just accept “we’ll give you the pill.”
- Don’t stop the medicine because of a fall. Talk to your doctor - don’t assume it’s too risky.
The truth is simple: for most seniors with atrial fibrillation, the risk of stroke is far greater than the risk of bleeding from a fall. Anticoagulants save lives. The question isn’t whether they’re safe - it’s whether we’re brave enough to use them.
What About Warfarin?
Warfarin still works. But it’s messy. You need blood tests every few weeks. Your diet matters. Alcohol changes how it works. It interacts with dozens of other drugs. For seniors, especially those living alone or with memory issues, it’s harder to manage safely. DOACs are simpler. They don’t need monitoring. They’re less affected by food or other meds. For most older adults, they’re the better choice - unless kidney function is very poor or cost is a barrier.Bottom Line
Falls are scary. Bleeding is scary. But not treating atrial fibrillation? That’s scarier. The data doesn’t lie: anticoagulants prevent more harm than they cause in seniors. The key isn’t avoiding the medicine - it’s managing the whole picture. Better kidney checks. Better fall prevention. Better conversations. If you’re over 65 and have an irregular heartbeat, don’t let fear of falling keep you from the treatment that could keep you alive - and independent - for years to come.Write a comment
Your email address will not be published.




11 Comments
Anticoagulants aren’t a panacea. The data you cite ignores real-world compliance, polypharmacy, and the fact that many elderly patients can’t swallow pills consistently-let alone remember to take them. Guidelines don’t account for dementia, wandering, or caregivers who forget to refill prescriptions. Just because a trial says ‘benefit’ doesn’t mean it translates to a 92-year-old living alone with three cats and no phone.
THEY’RE HIDING THE TRUTH!! 😡 Big Pharma doesn’t want you to know DOACs are just expensive placebos with hidden kidney damage! 🚨 The FDA’s been bought off since 2010, and your ‘studies’? All funded by Bristol-Myers Squibb. My cousin took apixaban and his urine turned green! 🤫 They’re covering it up! #PharmaLies #StopTheLies
Oh wow so falling is bad but stroke is worse? Shocking. Next you’ll tell me breathing is dangerous but drowning is worse. Maybe if we stopped giving old people medicine and let nature take its course, we’d save more money. 😏
This is so important ❤️ I’ve seen my grandma go from terrified of falling to actually enjoying walks after we did the Otago program. She’s 88 and still dances in the kitchen. It’s not about avoiding risk-it’s about managing it with love. Thank you for writing this!
YES. YES. YES. I’m a nurse and I’ve seen too many people on aspirin because ‘it’s safer’-and then they have a massive stroke. DOACs are game-changers. My 84-year-old patient started apixaban, got a fall prevention plan, and now he’s gardening again. Don’t let fear steal their life.
It is deeply troubling that medical practice remains so steeped in fear rather than evidence. The reluctance to prescribe anticoagulants to the elderly-despite overwhelming data-is not merely clinical negligence; it is a moral failure. We have, as a society, conflated the natural process of aging with vulnerability to the point of paternalistic abandonment. To withhold a life-saving intervention because someone might stumble is to prioritize convenience over dignity. The Hippocratic Oath demands we do no harm-and failing to act when the harm of inaction is quantifiably greater is the very definition of harm.
It is not the patient’s fall that is the crisis-it is the physician’s hesitation.
Interesting... but I wonder how many of these ‘24 strokes prevented vs 3 bleeds’ stats include people who had a fall, bled, and then died in the ER from a delayed response? The hospital data is clean, but the home data? Not so much. My neighbor’s dad took apixaban, slipped on the bathroom tile, and bled out before the ambulance got there. He was alone. No one knew. The ‘net benefit’ doesn’t account for lonely deaths.
While the statistical argument presented is compelling, it is imperative to recognize the epistemological limitations of population-level data when applied to individual clinical decision-making. The heterogeneity of geriatric physiology, the confounding variables of comorbidities, and the absence of longitudinal real-world adherence metrics render the generalization of ‘net benefit’ potentially misleading. A more nuanced, case-specific approach is warranted.
So... you’re saying we should just give old people blood thinners and hope they don’t fall? 😒 What about the ones who forget they’re on it and drink grapefruit juice? Or take ibuprofen? Or live in a house with 17 steps and no rail? This isn’t a pill problem-it’s a society problem. And we’re too lazy to fix it. So we just hand out anticoagulants and pretend we’re heroes.
They’re not trying to prevent strokes-they’re trying to keep the nursing homes full. 🤔 Think about it: if old people live longer, who pays for their care? Who profits? Hospitals? Pharma? The government? The system doesn’t want you to live independently-it wants you dependent. DOACs? More expensive. More paperwork. More profit. And if you bleed? Well, that’s just ‘natural causes’ on the death certificate. 💀 They want you on the pill... so you stay on the system.
Falls are preventable. Strokes are not. Stop being scared. Start being smart.