
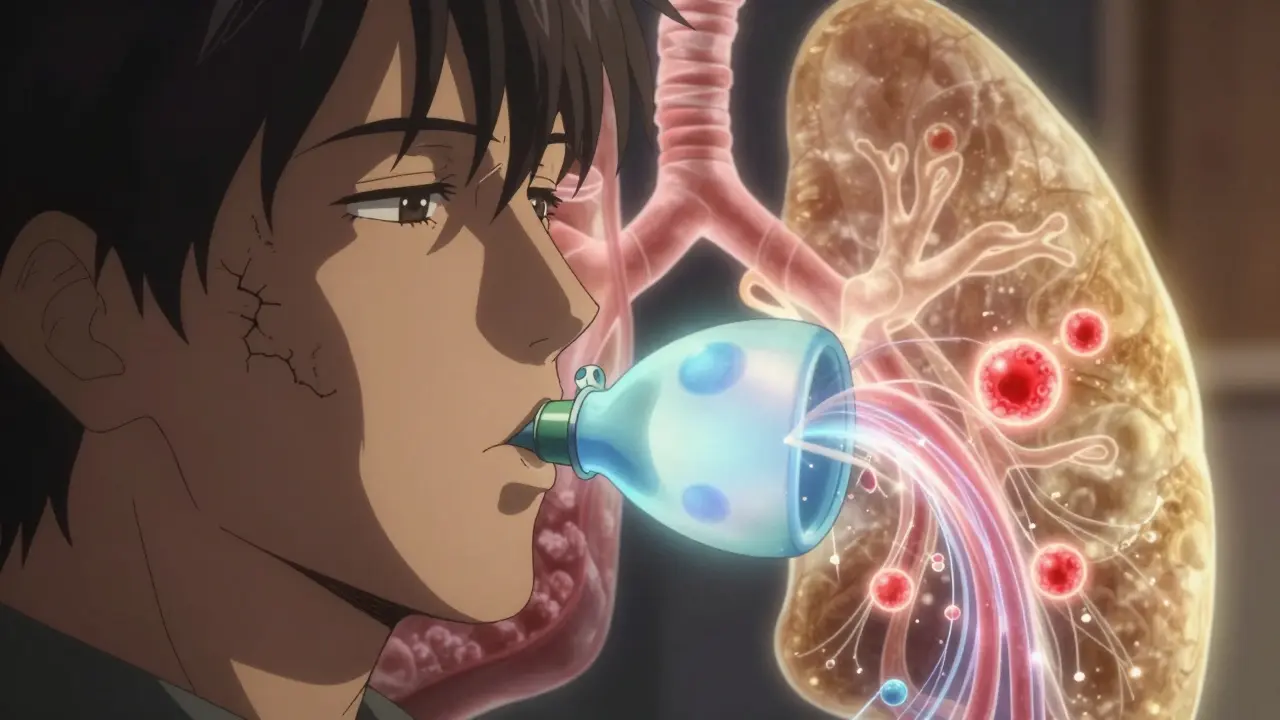
When your doctor orders pulmonary function tests, it’s not just another checkbox. These tests-especially spirometry and DLCO-can reveal what’s really going on in your lungs, even when you feel fine. Many people think if they can breathe okay, their lungs are fine. But that’s not always true. You could have early lung damage and still take a walk without getting winded. That’s why these tests matter. They don’t just measure air movement. They measure how well oxygen gets into your blood. And that’s the difference between feeling okay and being truly healthy.
What Spirometry Actually Measures
Spirometry is the most common lung test you’ll ever take. You breathe in as deep as you can, then blow out as hard and fast as you can into a tube connected to a machine. It sounds simple, but the numbers it gives you tell a detailed story.
The two key numbers are FEV1 and FVC. FEV1 is how much air you can blow out in the first second. FVC is the total amount you can blow out after one full breath. The ratio between them-FEV1 divided by FVC-is what doctors use to spot problems. If that ratio is below 0.7, you likely have airflow obstruction. That’s the hallmark of asthma or COPD. But if your ratio is normal and your FVC is low, that’s a different story. It suggests your lungs are stiff or your chest can’t expand fully. That’s restriction.
Here’s the catch: spirometry can’t tell you why your lungs are stiff. Is it from scar tissue? From being overweight? From a curved spine? That’s where DLCO comes in.
DLCO: The Hidden Key to Gas Exchange
DLCO stands for diffusing capacity of the lung for carbon monoxide. It sounds technical, but it’s really just measuring how well oxygen moves from your lungs into your blood. You inhale a tiny, harmless amount of carbon monoxide mixed with helium and oxygen. You hold your breath for 10 seconds-yes, exactly 10-and then exhale. The machine measures how much CO was absorbed. That tells you how efficiently your lungs transfer gas.
Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75% means your lungs aren’t moving oxygen well. Above 140%? That’s unusual, but it can happen with too many red blood cells, heart shunts, or even bleeding in the lungs.
Why does this matter? Because two people can have the same low FVC on spirometry, but totally different DLCO results. One might have pulmonary fibrosis-scar tissue in the lungs-and their DLCO will be very low. The other might be obese, and their DLCO will be normal. The first needs lung-specific treatment. The second needs weight management. Spirometry alone can’t tell them apart. DLCO can.
When DLCO Is Low and Spirometry Is Normal
This is one of the most overlooked patterns in clinical practice. You take the test. Your FEV1 and FVC are fine. Your ratio is normal. You walk out thinking, “I’m good.” But if your DLCO is low, you’re not.
A low DLCO with normal spirometry can mean several things:
- Early interstitial lung disease-like pulmonary fibrosis-before scarring is visible on scans
- Chronic pulmonary embolism-small blood clots blocking lung vessels
- Connective tissue diseases-like scleroderma or lupus-that quietly damage lung tissue
- Early emphysema-especially in smokers who haven’t lost much lung volume yet
Studies show DLCO can drop 12 to 18 months before spirometry changes. That’s a huge window to catch disease early. In fact, for people with idiopathic pulmonary fibrosis, a DLCO under 35% predicts a much higher risk of death. That’s why it’s used to decide who needs transplant evaluation.
When DLCO Is High
High DLCO isn’t common, but when it happens, it’s telling. In asthma, DLCO can rise to 120-140% during flare-ups because your lungs are overperfused and inflamed. In polycythemia-when your body makes too many red blood cells-there’s more hemoglobin to grab oxygen, so DLCO goes up. Left-to-right heart shunts (like a hole in the heart) pump extra blood through the lungs, also raising DLCO.
But here’s the trap: if you’re a smoker, your DLCO can be falsely low. Smoking raises carboxyhemoglobin, which competes with CO for binding sites. If your hemoglobin isn’t checked, you might be misdiagnosed with lung disease when you just need to quit smoking.
The FVC/DLCO Ratio: A Hidden Diagnostic Tool
Most doctors don’t use it. But the ratio of FVC to DLCO is one of the most powerful clues in lung diagnostics. If your FVC is normal but your DLCO is low, the ratio will be high. That’s normal. But if your FVC is low and your DLCO is even lower, the ratio might still be high-and that’s a red flag.
A ratio above 1.6 strongly suggests pulmonary hypertension. In fact, one study found this ratio was above 1.6 in 92% of patients with pulmonary arterial hypertension. That’s more reliable than some imaging tests. And it’s free-just from the same DLCO test you already had.

What Can Go Wrong With the Tests
Neither test is perfect. People struggle with the 10-second breath-hold for DLCO, especially older adults or those with anxiety. If you don’t hold long enough, the result is falsely low. If you exhale too fast or too slow during spirometry, your FEV1 gets messed up.
And here’s the biggest mistake: not checking hemoglobin. For every 1 gram per deciliter your hemoglobin drops, your DLCO drops about 1%. If you’re anemic, your DLCO looks worse than it is. If you’re polycythemic, it looks better. That’s why labs must report hemoglobin with DLCO results. If they don’t, ask for it.
Also, smoking within 24 hours before the test can lower DLCO by 5-10%. You don’t need to quit for good-but skip the cigarette that morning.
How These Tests Fit Into Real Diagnosis
Here’s how it usually plays out:
- You come in with shortness of breath. Your doctor orders spirometry.
- If FEV1/FVC is low? You likely have asthma or COPD. Bronchodilator test follows.
- If FEV1/FVC is normal but FVC is low? DLCO is next.
- If DLCO is low? Think fibrosis, embolism, or autoimmune disease.
- If DLCO is normal? Think obesity, chest wall deformity, or muscle weakness.
That’s it. No CT scan. No biopsy. Just two simple tests and a smart interpretation. And it works. A 2023 Mayo Clinic study showed AI models could predict pulmonary hypertension from DLCO patterns with 88% accuracy-just from the numbers.
Why This Matters for You
If you’ve been told your lungs are “fine” but you’re still tired or out of breath, ask about DLCO. Don’t accept a normal spirometry as the end of the story. Many people live for years with undiagnosed pulmonary fibrosis or chronic clots because no one checked DLCO.
And if you’re being monitored for a lung disease-like COPD, asthma, or fibrosis-DLCO isn’t optional. It’s the best way to track progression. A falling DLCO means your disease is worsening, even if your breathing feels the same. That’s when treatment needs to change.
This isn’t just for the elderly. People in their 30s and 40s with connective tissue disease or long-term asthma can have early lung damage. DLCO catches it before it’s too late.
What’s the difference between spirometry and DLCO?
Spirometry measures how much air you can move in and out of your lungs and how fast. DLCO measures how well oxygen moves from your lungs into your bloodstream. One looks at airflow; the other looks at gas exchange.
Can I have normal spirometry but still have lung disease?
Yes. Many early lung conditions-like pulmonary fibrosis, chronic pulmonary embolism, or early emphysema-don’t affect airflow right away. They damage the tiny air sacs and blood vessels where oxygen enters the blood. That’s what DLCO detects. Normal spirometry doesn’t mean healthy lungs.
Why is hemoglobin checked with DLCO?
Hemoglobin carries oxygen in your blood. If your hemoglobin is low (anemia), less oxygen can be transported, making DLCO appear lower than it really is. If it’s high (polycythemia), DLCO looks artificially high. The test result must be corrected for your actual hemoglobin level to be accurate.
Does smoking affect DLCO results?
Yes. Smoking increases carboxyhemoglobin in your blood, which competes with the carbon monoxide used in the test. This can falsely lower your DLCO by 5-10%. You should avoid smoking for at least 24 hours before the test.
What does a low DLCO with normal spirometry mean?
It suggests a problem with gas exchange, not airflow. Common causes include early interstitial lung disease, chronic pulmonary embolism, connective tissue disorders, or early emphysema. This pattern often needs further testing like a CT scan or blood tests for autoimmune markers.
Is DLCO testing painful or risky?
No. You inhale a tiny, safe amount of carbon monoxide-far less than what’s in a cigarette. You hold your breath for 10 seconds. It’s non-invasive and carries no risk. Some people feel lightheaded briefly, but that’s rare and passes quickly.
How often should DLCO be repeated?
For monitoring diseases like pulmonary fibrosis or COPD, it’s typically done every 6 to 12 months. For unexplained shortness of breath, it’s usually a one-time test unless results are unclear or symptoms change. Your doctor will decide based on your condition.
Write a comment
Your email address will not be published.


14 Comments
I never realized how much DLCO matters until my doctor ordered it after I kept feeling tired. My spirometry was normal, but DLCO was low. Turns out I had early pulmonary fibrosis. Don't let normal numbers fool you.
This is so important! 🙌 I'm a nurse and I've seen so many patients get dismissed because their spirometry looked fine. DLCO is the silent hero of lung diagnostics. Everyone should ask for it if they're still breathless.
You people overcomplicate everything. In India we just treat symptoms. If you cant breathe you get inhaler. Why waste time on fancy numbers
This post changed how I talk to my patients. I used to stop at spirometry. Now I always check DLCO and hemoglobin. It’s not just better medicine-it’s more compassionate. People deserve to know what’s really going on.
I had a low DLCO once and thought I was dying. Turned out I was anemic. Got iron pills and now I’m fine. Just shows how much context matters. Don’t panic at one number.
It’s funny how we think health is about what we can feel. But the body hides so much. DLCO is like a whisper from your lungs saying ‘pay attention’. Most of us only listen when it’s screaming.
I’ve been pushing this in my clinic for years. If you’re a smoker and your DLCO is low, check your hemoglobin first. So many people get misdiagnosed because no one checks the basics.
Americans overtest everything. In my country we don't need fancy machines. Just tell them to stop smoking and move more. Problem solved.
The FVC/DLCO ratio >1.6 as a predictor for PAH is wild. I’ve started using it in my pulmonology rotations. It’s a game-changer for early detection. No imaging needed. Just math and physiology.
As a medical educator, I emphasize this exact framework in my lectures. The elegance lies in its simplicity: two tests, one algorithm, and a profound diagnostic yield. It’s evidence-based medicine at its finest.
You people need to stop using 'DLCO' like it's some mystical incantation. It's just a test. And if you're not correcting for hemoglobin, you're doing it wrong. And smoking? Of course it affects it. That's not news.
Fascinating. Though I suspect most American clinicians still don't know how to interpret it properly. The gap between knowledge and practice remains vast.
This is gold. I work in a rural clinic and we dont always have CT scans. DLCO is our best friend. Just need to make sure the machine is calibrated and the patient understands the breath hold. Small things matter.
The 2023 Mayo Clinic AI study is compelling. But we must remember: algorithms support, not replace, clinical judgment. The numbers are tools-not truths. Always correlate with history and physical.