Think you have a bad case of stomach bugs or food intolerance? Maybe it’s not just a bad meal. If you’re dealing with constant bloating, cramps, or changes in bowel habits, you’re not alone. But here’s the thing: not all gut problems are the same. Two conditions that look almost identical on the surface - IBS and IBD - are actually worlds apart in how they work, how they’re diagnosed, and how they’re treated. Mixing them up can lead to the wrong care, unnecessary stress, or even missed danger signs.
What Is IBS, Really?
IBS stands for Irritable Bowel Syndrome. It’s not an infection. It’s not cancer. And it doesn’t show up on scans or blood tests. That’s why it’s called a functional disorder - your gut looks normal, but it just doesn’t work right.
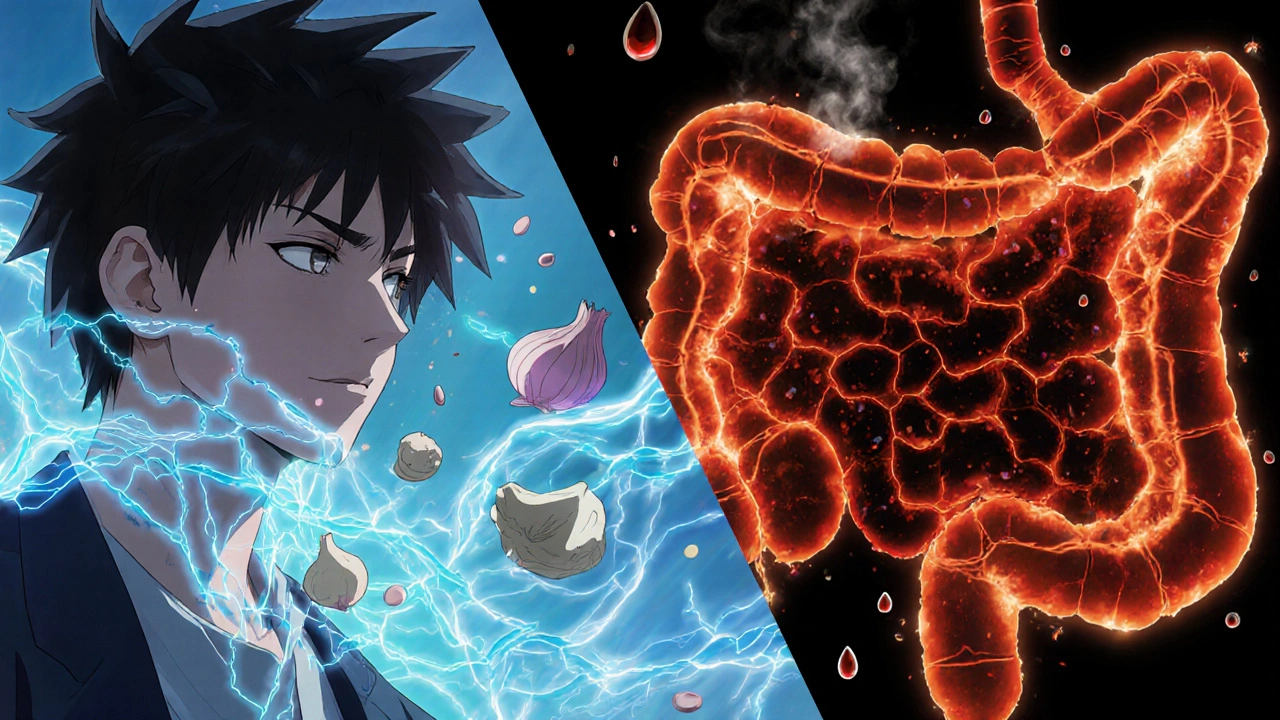
People with IBS often feel pain or discomfort at least once a week for three months or more. That pain usually gets better after a bowel movement. You might also notice bloating, gas, mucus in your stool, or your bowel habits switching between diarrhea and constipation. About 76% of people with IBS report bloating, and nearly half see mucus in their stool. It’s common for symptoms to flare up after eating, especially with certain foods like onions, garlic, beans, or dairy.
The big surprise? No one knows exactly what causes IBS. But it’s not your fault. It’s linked to how your brain and gut talk to each other. Stress, past infections, and even your gut bacteria can play a role. The good news? IBS doesn’t damage your intestines. It doesn’t lead to cancer. It doesn’t require surgery. And while it’s lifelong for many, it doesn’t get worse over time.
What Is IBD, and Why It’s More Serious
IBD - Inflammatory Bowel Disease - is something else entirely. It’s not just "irritated" bowels. It’s chronic inflammation that eats away at your digestive tract. There are two main types: Crohn’s disease and ulcerative colitis.
Crohn’s can hit anywhere from your mouth to your anus, causing patches of deep inflammation. Ulcerative colitis sticks to the colon and rectum, creating continuous sores and ulcers. Unlike IBS, IBD shows up clearly on tests. Endoscopies reveal open wounds. Biopsies show inflamed tissue. Blood tests show elevated markers like CRP and fecal calprotectin - signs your body is fighting an internal war.
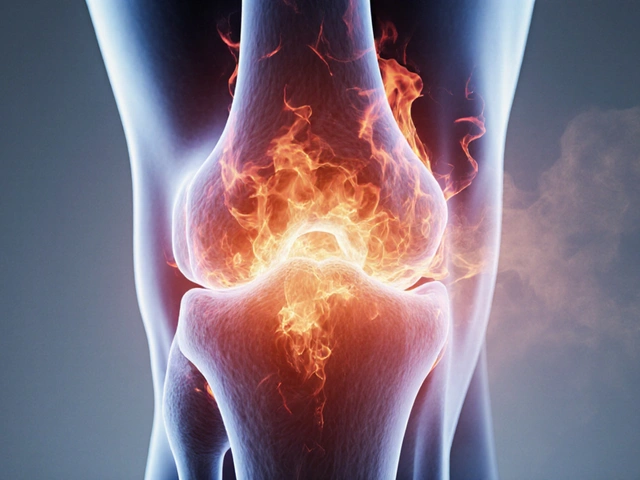
And the symptoms? They go beyond cramps and bloating. People with IBD often have bloody stools - red or dark, tarry bowel movements. They lose weight without trying. They get fevers. Some develop joint pain, skin rashes, or eye inflammation. These aren’t "side effects." They’re part of the disease. About 20-30% of IBD patients get arthritis. Around 10% get painful red bumps on their shins called erythema nodosum. These are signs your immune system is attacking more than just your gut.
IBD can lead to life-threatening complications. Strictures - narrowings in the intestine - can block food. Fistulas - abnormal tunnels between organs - can cause infections. And long-term IBD increases your risk of colon cancer. After 10 years of full-colon involvement, the risk jumps by 2% each year. That’s why regular monitoring isn’t optional. It’s necessary.
The Key Difference: Damage vs. Dysfunction
Here’s the simplest way to tell them apart: IBS is a software glitch. IBD is hardware damage.
With IBS, your gut’s wiring is misfiring. The muscles contract too hard or too weak. Your nerves are overly sensitive. Everything looks normal under the scope - no swelling, no ulcers, no bleeding. Tests come back clean. That’s why doctors diagnose IBS by ruling everything else out.
With IBD, your immune system is on a rampage. It attacks your intestinal lining. You get real, visible damage. Ulcers. Inflammation. Scarring. These changes show up on colonoscopies, MRIs, and biopsies. Blood and stool tests catch the inflammation before you even feel it.
One of the biggest red flags? Blood in your stool. If you’re seeing bright red blood or black, tarry stools, that’s not IBS. That’s IBD - or something else serious. And if you’re losing weight without trying, running fevers, or feeling constantly tired, those are alarm bells. IBS doesn’t cause those. IBD does.

How Doctors Diagnose Each One
Diagnosing IBS is like solving a puzzle with missing pieces. There’s no single test. Doctors use the Rome IV criteria: abdominal pain at least once a week for three months, linked to bowel movements, and changes in stool frequency or form. Then they check for "alarm features": unexplained weight loss, rectal bleeding, family history of colon cancer, or anemia. If those are absent, and standard tests come back normal, IBS is likely.
Diagnosing IBD? That’s a full investigation. You’ll likely get blood work to check for inflammation. Stool tests to rule out infections. A colonoscopy - where a camera goes into your colon - to look for ulcers and take tissue samples. Sometimes you’ll need an MRI or CT scan to see deeper into your intestines, especially if Crohn’s is suspected. The biopsy results are key. If your pathologist sees chronic inflammation, crypt abscesses, or granulomas, that’s IBD.
Here’s the catch: you can have both. About one in three people with IBD in remission still meet the criteria for IBS. Their gut is healed, but their nerves are still on edge. That’s why it’s so important to get the right diagnosis upfront.
Treatment: Fixing the System vs. Calming the Fire
IBS treatment is about managing triggers and retraining your gut. Diet changes are the first line. The low-FODMAP diet helps 76% of people reduce bloating, pain, and diarrhea. That means cutting back on certain sugars found in wheat, onions, apples, and dairy. It’s not forever - you reintroduce foods slowly to find your triggers.
Medications help too. Low-dose antidepressants like amitriptyline can calm overactive nerves in the gut. Drugs like eluxadoline or linaclotide target specific symptoms. Stress management - through therapy, yoga, or mindfulness - often makes a bigger difference than people expect.
IBD treatment is about stopping the immune system’s attack. You need powerful drugs. Anti-TNF biologics like infliximab shut down inflammation and put about half of Crohn’s patients into remission within 14 weeks. Steroids like prednisone work fast for flares but aren’t safe long-term. Newer drugs like vedolizumab target only the gut, reducing side effects. Some people need surgery to remove damaged parts of the intestine.
There’s no cure for either condition. But IBD treatment can stop progression. IBS treatment can bring relief. The goals are different - and so are the tools.

Can IBS Turn Into IBD?
No. This is a myth that causes unnecessary fear. IBS does not turn into IBD. They are completely different diseases with different causes. One is a functional disorder. The other is an autoimmune disease.
But you can have both at the same time. If you’ve been diagnosed with IBD and still have gut symptoms even when your inflammation is under control, you might also have IBS. That’s why doctors now screen for IBS in IBD patients in remission. It’s not a progression - it’s a coexistence.
When to See a Doctor - Right Now
Not every stomach ache needs a hospital visit. But if you have any of these, don’t wait:
- Bloody or black stools
- Unexplained weight loss
- Constant fever
- Severe, persistent pain that wakes you up at night
- Family history of colon cancer or IBD
- Anemia or fatigue that won’t go away
These aren’t "IBS symptoms." They’re signs your body is fighting something serious. Delaying care can lead to complications you can’t undo.
Living With It
Both IBS and IBD change your life. People with IBS say they’d give up caffeine, their phone, even sex to be free of symptoms. That’s how much it affects daily living. IBD patients face hospital stays, infusions, and surgeries. Both can make you feel isolated.
But knowledge is power. Knowing whether you have IBS or IBD helps you make smarter choices - what you eat, how you manage stress, when to push for tests, and when to ask for help. It takes the guesswork out of your health.
Bottom line: IBS is frustrating. IBD is dangerous. But both are manageable. And you don’t have to figure it out alone. Get the right diagnosis, work with your doctor, and take control - one step at a time.
Can IBS turn into IBD?
No, IBS cannot turn into IBD. They are completely different conditions. IBS is a functional disorder with no structural damage, while IBD is an autoimmune disease that causes inflammation and physical damage to the gut. One does not progress into the other. However, it’s possible to have both at the same time - especially if you have IBD in remission but still experience gut symptoms like bloating or cramping.
Is blood in my stool a sign of IBS?
No, blood in the stool is not a symptom of IBS. If you see red blood in your toilet, on toilet paper, or in your stool, that’s a red flag for IBD, infection, hemorrhoids, or another serious condition. IBS does not cause bleeding. Any rectal bleeding should be evaluated by a doctor immediately - don’t assume it’s just IBS.
Do I need a colonoscopy to diagnose IBS?
Not always, but it’s often used to rule out IBD or other conditions. IBS is diagnosed by excluding other diseases. If you’re under 50, have no family history of colon cancer, and have no alarm symptoms like bleeding or weight loss, a colonoscopy might not be needed. But if you’re over 50, have risk factors, or symptoms are new or worsening, your doctor will likely recommend one to make sure it’s not IBD or something else.
Can diet cure IBD?
No diet can cure IBD. While certain diets like low-FODMAP or exclusive enteral nutrition can help manage symptoms and support healing, they don’t stop the underlying inflammation. IBD requires medical treatment - usually anti-inflammatory or immune-suppressing drugs. Diet is a tool for symptom control, not a replacement for medication.
Are stress and anxiety the cause of IBS?
Stress and anxiety don’t cause IBS, but they can make it worse. IBS is linked to how your brain and gut communicate. If your nervous system is on high alert, your gut becomes more sensitive. That’s why therapies like cognitive behavioral therapy (CBT) and mindfulness help - they calm the brain-gut connection. But the root cause is likely a mix of genetics, gut bacteria, and past infections, not just stress.
Can IBD be managed without medication?
For most people, no. IBD is a chronic autoimmune disease that causes ongoing inflammation. Without medication, that inflammation can lead to permanent damage, strictures, fistulas, or cancer. While diet, rest, and stress management help, they’re not enough to control the disease. Medications like biologics or immunomodulators are necessary to stop the immune system from attacking your gut.
What’s the difference between IBD and IBS in terms of cancer risk?
IBS carries no increased risk of colon cancer. IBD, however, does. After 10 years of having ulcerative colitis that affects your entire colon, your risk of colorectal cancer increases by about 2% per year. That’s why regular colonoscopies with biopsies are part of long-term IBD care. Monitoring helps catch precancerous changes early.
Is IBS more common than IBD?
Yes, by a large margin. IBS affects 10-15% of people worldwide - that’s about 1 in 7 people. IBD affects about 1.3% of the U.S. population - roughly 1 in 75. IBS is far more common, but IBD is more serious. Because IBS is so widespread, many people assume all gut problems are just "IBS," which can delay diagnosis of IBD and lead to dangerous consequences.
Write a comment
Your email address will not be published.



11 Comments
Man, I wish I’d read this five years ago. I spent a year thinking my IBS was just "bad digestion" until I started bleeding and ended up in the ER. Turns out it was Crohn’s. IBS doesn’t make you lose 20 pounds in a month or wake up with a fever. This post nailed it - functional vs. broken. Don’t ignore the red flags.
It is deeply concerning that so many individuals continue to conflate these two entirely distinct pathological entities. The casual dismissal of inflammatory bowel disease as mere "irritability" is not only medically inaccurate, but potentially life-threatening. One must exercise rigorous diagnostic discipline.
IBS and IBD... both real. But I’ve seen people in India told "it’s just stress" for years. Then they end up with fistulas. No tests, no doctors, just chai and prayers. This post should be translated. People need to know - bleeding isn’t normal. Weight loss isn’t "just dieting".
ok but like… why do they even have the same acronym?? IBS? IBD? sounds like a typo. i had both and the doc just said "you got the bad one". i lost my colon. also low fodmap is a scam if you’re not rich. i eat ramen now and it’s fine. also why are there so many questions at the bottom like a FAQ page???
This is an exceptionally well-structured and clinically accurate exposition. The distinction between functional dysregulation and structural inflammation is articulated with clarity and compassion. I will be sharing this with my patients who often self-diagnose based on internet forums. Thank you for the precision and care in this piece.
Biggest thing I learned? IBS doesn’t cause weight loss or fevers. I thought I was just "sick all the time" - turns out I had ulcerative colitis. I was misdiagnosed for 3 years. If you’re losing weight or bleeding, don’t wait. Get the colonoscopy. Your future self will thank you.
Excellent breakdown. The software vs. hardware analogy is perfect. IBS is like a glitchy app - frustrating, but your phone still works. IBD is like a cracked motherboard - you need repairs before it dies. And yes, blood in the stool? That’s not "gas." That’s a red flag. Get it checked.
They’re hiding something. Why does Big Pharma push biologics for IBD but only tell IBS people to "eat less beans"? IBS is a cover-up. The real cause is glyphosate in the food supply and 5G messing with your vagus nerve. I know people who healed with lemon water and earthing mats. They don’t want you to know this. IBD? That’s just the distraction. Look at the research - it’s all funded by pharma. The bleeding? It’s the toxins. The weight loss? The suppression. Wake up.
IBS not IBD no blood no weight loss no fever no cancer risk. If you got all that its IBD. Done.
My cousin was told she had IBS for 7 years. Then she collapsed. Turned out she had Crohn’s with a perforation. She needed emergency surgery. If you’re tired all the time and your stomach hurts after everything - don’t just live with it. Push for tests. This post saved my life. Seriously.
IBS doesn’t cause bleeding. IBD does. Get checked if you’re losing weight or have fevers. Don’t wait.