
Opioid Withdrawal Timeline Calculator
Enter the type of opioid and time of last use to see the expected withdrawal timeline.
Withdrawal Timeline Estimate
Based on your inputs:
Note: Individual experiences vary based on factors like dosage, duration of use, and overall health. This is a general estimate only.
Understanding Your Timeline
Withdrawal timelines differ based on opioid type:
- Short-Acting Opioids (heroin, oxycodone, hydrocodone): Symptoms typically begin 8-12 hours after last use, peak at 48-72 hours, and resolve within 7-10 days.
- Long-Acting Opioids (methadone, extended-release morphine): Symptoms may not appear until 24-36 hours after last use, peak around 72 hours, and can last 14 days or more.
Medical supervision during withdrawal reduces complications and improves outcomes. Consider discussing treatment options with a healthcare professional.
Opioid Withdrawal is a physiological syndrome that occurs when a person who has developed physical dependence on opioids abruptly reduces or stops use. It triggers a predictable set of physical and psychological symptoms that follow a clear temporal pattern. Understanding the opioid withdrawal timeline helps clinicians and patients plan safer detoxification and reduces the chance of relapse.
What Happens During Opioid Withdrawal?
The body reacts to the sudden loss of opioid stimulation with a cascade of autonomic and neuro‑chemical changes. Common signs include lacrimation, runny nose, goose‑flesh, muscle aches, nausea, vomiting, diarrhea, dilated pupils, yawning, sweating, rapid heart rate, and insomnia. Psychological effects such as anxiety, irritability, and depression often appear early and can linger after the physical symptoms subside.
Timeline: Short‑Acting vs. Long‑Acting Opioids
Withdrawal timing depends heavily on the opioid’s half‑life.
- Short‑acting opioids (heroin, immediate‑release oxycodone, hydrocodone): symptoms start 8‑12 hours after the last dose, peak at 48‑72 hours, and usually resolve within 7‑10 days.
- Long‑acting opioids (methadone, extended‑release morphine): symptoms may not appear until 24‑36 hours, peak around 72 hours, and can last 14 days or more.
Clinicians often break the course into three phases (early 6‑24 h, peak 72 h, final week) to match treatment intensity with symptom severity.
Assessing Severity: The COWS Tool
Clinical Opioid Withdrawal Scale (COWS) is an 11‑item rating system that quantifies withdrawal intensity from 0‑47. Scores guide whether a patient needs outpatient monitoring (5‑12), moderate intervention (13‑24), or inpatient management (25+). Regular COWS checks-every 2‑4 hours during acute withdrawal-ensure medication doses are adjusted promptly.
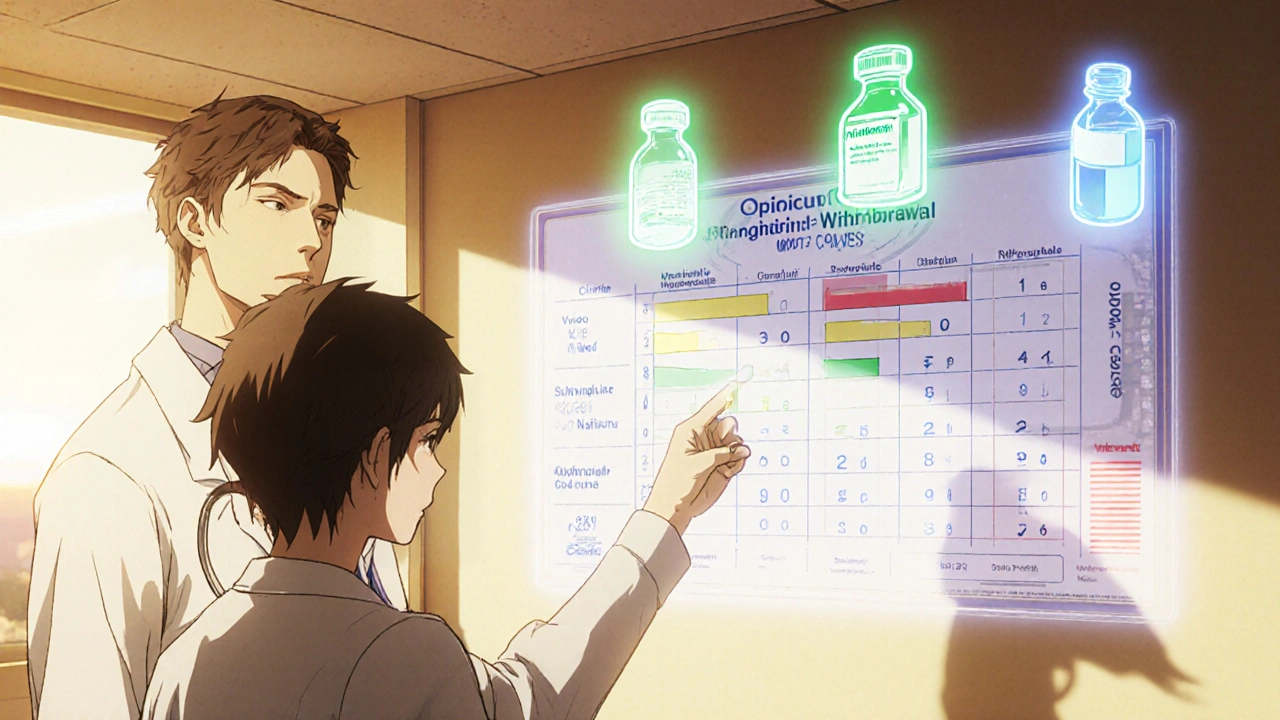
Pharmacologic Management
Medically supervised detox uses three FDA‑approved options. The choice depends on opioid history, setting, and patient preference.
| Medication | Onset | Half‑life | Typical Dose | Reduction in Withdrawal Severity |
|---|---|---|---|---|
| Methadone | 30‑60 min | 24‑36 h | 20‑40 mg/day | ≈70 % |
| Buprenorphine | 15‑30 min | 36‑60 h | 2‑8 mg/day | ≈65‑70 % |
| Naltrexone | 1‑2 h (after opioid‑free period) | 4‑6 h | 50 mg daily | Prevents relapse, does not relieve acute symptoms |
Buprenorphine’s partial agonist profile makes it especially effective at cutting cravings while producing a ceiling effect on respiratory depression. Methadone offers smoother tapering for long‑term users but requires daily clinic visits in many jurisdictions. Naltrexone is used after detox to block opioid receptors and reduce overdose risk.
Non‑Pharmacologic Strategies
Medication alone rarely addresses the whole picture. Complementary measures improve comfort and keep patients hydrated.
- Hydration Therapy: Offer 2‑3 L of oral rehydration solution daily to offset fluid loss from vomiting and diarrhea. Electrolyte replacement (sodium, potassium) prevents dangerous imbalances.
- Nutrition: Light, high‑protein meals and vitamin B complex support metabolic recovery.
- Cognitive Behavioral Therapy (CBT): Sessions focused on anxiety, cravings, and coping skills reduce relapse rates by up to 30 % when paired with medication.
- Acupuncture: A 2019 meta‑analysis showed a 25‑30 % reduction in withdrawal severity for two‑thirds of participants.
Designing a Tapering Protocol
For prescribed‑opioid users, a gradual reduction minimizes withdrawal peaks. A typical Tapering Protocol reduces the daily dose by 10‑20 % every 3‑7 days, extending the overall taper to 4‑8 weeks for chronic users. Example for oxycodone 30 mg daily:
- Day 1‑7: 27 mg (10 % reduction)
- Day 8‑14: 24 mg
- Continue until 5 mg, then switch to a short‑acting opioid for final weeks.
Frequent COWS assessments guide whether the reduction needs to pause or slow down.
Risks, Complications, and Post‑Detox Planning
While opioid withdrawal itself isn’t usually life‑threatening for healthy adults, complications can arise:
- Severe dehydration and electrolyte imbalance (12‑15 % of unsupervised withdrawals).
- Cardiac stress from prolonged tachycardia.
- Elevated overdose risk-tolerance drops sharply, making any post‑detox use far more dangerous (3‑5 × higher fatality in the first month).
Therefore, discharge planning should include immediate entry into medication‑assisted treatment (MAT) or intensive outpatient counseling. Evidence shows a 40‑60 % success rate for patients who stay on buprenorphine or methadone for 6‑12 months after detox.
Key Takeaways
- Withdrawal timing hinges on opioid half‑life: 8‑12 h onset for short‑acting, 24‑36 h for long‑acting.
- Peak severity hits around 48‑72 h; most physical symptoms fade by day 7‑10, but mood disturbances may linger.
- Use COWS to monitor severity and tailor medication doses.
- Methadone, buprenorphine, and naltrexone are the three FDA‑approved pharmacologic tools; buprenorphine offers the best balance of safety and symptom relief.
- Combine meds with hydration, nutrition, CBT, and possibly acupuncture for a smoother experience.
- Implement a structured taper (10‑20 % reduction every 3‑7 days) for prescription opioid users.
- Plan for ongoing MAT or counseling to cut the high post‑detox overdose risk.
Frequently Asked Questions
How quickly do withdrawal symptoms start after stopping heroin?
Symptoms usually appear within 6‑12 hours, with the worst intensity around 48‑72 hours.
Can I go through withdrawal at home without medication?
Home detox is possible for mild cases, but the risk of dehydration and severe electrolyte loss is high. Medical supervision dramatically improves completion rates.
What is the difference between methadone and buprenorphine?
Methadone is a full opioid agonist with a longer half‑life, requiring daily clinic dosing in many places. Buprenorphine is a partial agonist, offers a ceiling effect on respiratory depression, and can be prescribed for take‑home use.
How does the Clinical Opioid Withdrawal Scale work?
COWS scores 11 signs (e.g., pupil size, sweating, tremor) on a 0‑4 scale. The total score categorizes withdrawal as mild, moderate, or severe, guiding treatment intensity.
Is acupuncture really effective for opioid withdrawal?
A 2019 meta‑analysis reported a 25‑30 % reduction in symptom severity for most participants, making it a useful adjunct, especially when medication access is limited.
Write a comment
Your email address will not be published.





10 Comments
People think they can trust the official timelines but the pharma giants have been tweaking the data for decades. They hide how long the cravings actually last because longer pain means more profit. The withdrawal curve is a tool they use to keep us dependent. If you look at the half‑life numbers you’ll see a pattern that matches their marketing cycles. Notice how the short‑acting opioids are praised while the long‑acting ones get extra scrutiny. That can’t be a coincidence when you consider the lobbying power behind methadone clinics. The guide mentions COWS scores but doesn’t warn about how the scale can be used to justify higher doses of medication that keep the pocket‑book happy. Every time a patient improves, the report pushes a new “protocol” that adds another layer of control. Remember that the “non‑pharmacologic” tips are just a veneer to make the whole package look holistic while the real money stays in the pills. The timeline itself is a narrative engineered to keep you in the system longer than you need to be.
Thanks for pointing that out, it’s a reminder to stay critical of the sources 😊. While the big picture can feel overwhelming, the practical steps in the guide-like staying hydrated and using COWS to gauge severity-are solid tools that many clinicians rely on. A well‑structured taper combined with supportive counseling can actually break that cycle you mentioned. Keep an eye on how each recommendation aligns with evidence‑based practice, and don’t let the noise drown out the useful bits.
Oh great, another glossy hand‑out that pretends opioid withdrawal is just a week‑long flu. As if a simple table of meds can solve the decades‑long trauma of addiction. The tone feels like a corporate brochure written by someone who never saw a desperate patient in a cold ER.
Sure, because the real problem is that people don’t follow a chart. Maybe if the guide mentioned how cultural stigma prevents folks from seeking help it would be more useful. Instead we get a bullet list that sounds like a recipe for a sitcom.
Yo, this guide is like a mixtape of pharma hype and half‑baked life hacks. The meds listed are the usual suspects, but the real scoop is how the system rigs the game to keep us buying the next line. If you’re looking for a straight‑up strategy, skip the corporate fluff and focus on staying hydrated, eating real food, and finding a therapist who actually gives a damn about your story. And don’t be fooled by the “aggressive” language they use to scare you into compliance-real recovery is about patience, not panic.
Wow, that hit me right in the feels!
Honestly, the guide does a decent job of laying out the basics, but let’s be real-everyone’s journey is unique. The supportive tone is welcome, yet it can’t replace the empathy you get from a lived‑in experience. If you’re feeling stuck, reach out to a peer group that’s walked this path; they’ll understand the nuances that a chart can’t capture.
When I first read through the withdrawal timeline I thought it was just another dry medical pamphlet, but then the reality of each sentence began to unfold like a tragic opera. The first hour after the last dose feels like a slow‑burning candle that flickers in the dark, each breath a whisper of the battle to come. By the second day the body erupts in a chorus of symptoms-sweat, tears, tremors-a cacophony that seems almost theatrical in its intensity. The guide mentions that peak severity hits around 48‑72 hours, and that is precisely when the internal storm reaches its crescendo, a relentless tide that threatens to wash away any semblance of calm. Yet within that chaos, a glimmer of hope appears in the form of medication‑assisted treatment, a lifeline that can anchor the frantic heart. Methadone and buprenorphine are described not just as drugs but as characters in this drama, each with a distinct role-one a steady, long‑lasting presence, the other a quick‑acting hero with a ceiling that protects against the darkest ends. The narrative then turns to non‑pharmacologic measures, a surprising intermission where hydration and nutrition take the stage, reminding us that the simplest acts can be the most restorative. Acupuncture, for instance, is portrayed as a subtle, almost mystical chord that can ease the dissonance of withdrawal, offering a nuanced counterpoint to the more overt pharmacology. As the days stretch into a week, the physical symptoms begin to wane, but the psychological echo lingers like a lingering after‑taste, urging continuous support and counseling. The guide wisely stresses the importance of post‑detox planning, because without a solid script for the next act, the risk of relapse looms like an ominous shadow. The final takeaway resonates like the closing line of a powerful ballad: recovery is not a solo performance but a collaborative symphony of medication, therapy, and personal resilience. In the end, the timeline is not just a schedule but a map of transformation, guiding those who dare to walk its winding roads toward a horizon of renewed possibility.
Stay positive folks, the protocol is just a framework you can tweak with the right energy and support vibes. Hydration is your best friend, electrolytes keep the cells humming, and CBT gives the brain a fresh reboot. Even if the guide sounds clinical, the underlying message is simple: keep moving, stay connected, and trust the process.
Appreciate the depth of the long comment, it really captures the emotional roller coaster. Just a heads‑up, remember to pace yourself and not overcommit to every aggressive suggestion-balance is key. Focus on the practical steps that fit your schedule while keeping the big picture in mind.