
Every year, over a million people in the U.S. are harmed by medication errors - and many of these mistakes happen right at the pharmacy counter. You might think your doctor wrote the right prescription and the pharmacist filled it correctly. But that’s not always true. A wrong dose, the wrong pill, or even someone else’s medication can end up in your hands. The good news? You don’t have to just take it on faith. Verifying your prescription is your last, best chance to catch an error before you leave the pharmacy.
Check Your Name and Date of Birth First
Before you even look at the bottle, confirm the name on the label matches your legal name exactly. Not your nickname. Not your middle name. Your full legal name. Same with your date of birth. These are the two official patient identifiers every pharmacy is required to use. I’ve seen cases where a 72-year-old woman got her neighbor’s diabetes pills because the pharmacist mixed up two patients with similar last names. Both had the same first name. Both were in their 70s. Both had prescriptions filled on the same day. The error was caught only because the woman asked, “Why does this pill look different?”
Match the Medication Name to What Your Doctor Said
Does the name on the label match what your doctor told you? Don’t assume the generic version is the same as the brand. Sometimes they’re different - not in effectiveness, but in appearance. For example, metformin (generic) might look completely different from Glucophage (brand). If your doctor said you’d get “amoxicillin 500mg,” but the label says “amoxicillin 875mg,” stop. That’s a 75% overdose. Dosage errors are the most common type of pharmacy mistake, making up nearly one-third of all reported errors. If the name doesn’t match, ask the pharmacist to double-check the original prescription.
Look at the Strength and Form
Is it a tablet? A capsule? A liquid? Is it 5mg, 10mg, or 25mg? The strength matters just as much as the name. A patient once received 10mg of lisinopril instead of 5mg - thinking it was the same pill because the bottle looked familiar. He ended up in the ER with dangerously low blood pressure. The label said “lisinopril 10mg,” but his doctor prescribed 5mg. He didn’t check. Don’t be that person. Hold the bottle up to the light. Read the strength printed on the label. If it’s a liquid, check if it’s 5mg per 5mL or 5mg per mL. That’s a tenfold difference.
Count the Pills or Measure the Liquid
Don’t just grab the bottle and walk out. Count the pills. If your prescription says 30 tablets, count them. If it’s 60, count them all. You’d be surprised how often pills are missing - 9% of all pharmacy errors involve the wrong quantity. One woman picked up her thyroid medication and didn’t notice 10 pills were missing until she ran out two weeks early. She went back, and the pharmacist admitted they’d accidentally pulled the wrong bottle. If it’s a liquid, check the volume. Is it 100mL or 50mL? Use your phone’s camera to zoom in if the print is too small.

Read the Instructions Out Loud
“Take one by mouth daily.” Sounds simple. But what does “daily” mean? Morning? Night? With food? On an empty stomach? Is it “take as needed” or “take every 6 hours”? Ambiguous instructions cause nearly 20% of medication errors. If the label says “take 1 tab PO qd,” ask what “qd” means. Don’t guess. Pharmacists are trained to explain these abbreviations. If they roll their eyes or say, “It’s standard,” that’s a red flag. Write it down. Say it out loud: “I take one white tablet every morning with breakfast.” If it doesn’t sound right, ask again.
Check the Expiration Date and Packaging
Expired medication doesn’t just lose effectiveness - it can become dangerous. The FDA has tracked cases where patients took expired antibiotics and developed resistant infections. Look at the expiration date on the bottle. Is it more than a year away? If it’s less than six months, ask if they have a fresher batch. Also, check the packaging. Is the seal broken? Is the bottle cracked? Are the pills discolored or crumbling? If the bottle smells funny - like vinegar or mold - don’t take it. Four percent of recalled medications reach patients because of expired or damaged packaging. Don’t let that be you.
For Controlled Substances, Ask About the Prescription
If you’re getting opioids, sleeping pills, ADHD meds, or other controlled substances, the rules are stricter. Pharmacists are required to verify your address and confirm the prescription is legitimate. But they can’t do that if you don’t speak up. Ask: “Is this prescription valid?” or “Did my doctor call this in?” If they seem hesitant or avoid eye contact, that’s not normal. You have the right to know. And if you’re picking up someone else’s controlled substance - like a child’s or parent’s - make sure you’re authorized. Pharmacies are required to check this.
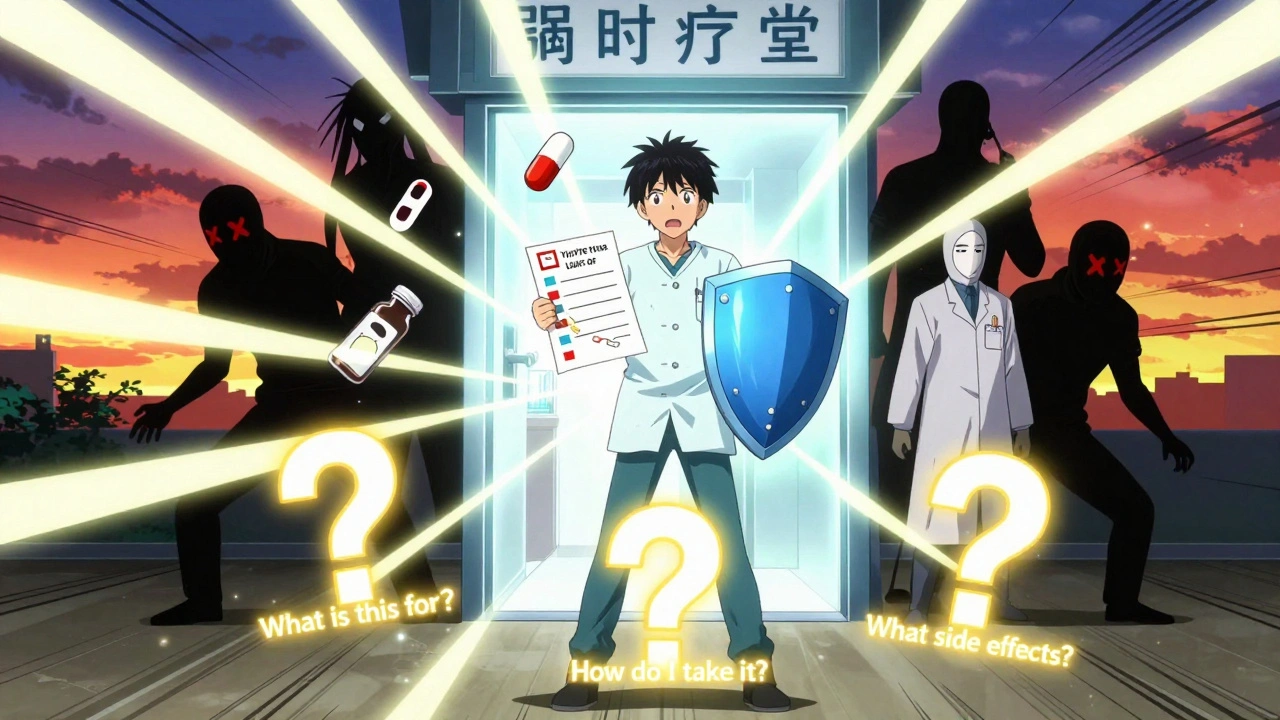
Ask the Three FDA Questions
The FDA says every patient should ask these three things before leaving the pharmacy:
- What is this medication for?
- How and when should I take it?
- What side effects should I watch for?
If the pharmacist can’t answer these clearly, walk out and call your doctor. You’re not being difficult - you’re being smart. Studies show patients who ask these questions catch 65% of potential errors before leaving the pharmacy.
What If You Spot an Error?
Don’t apologize. Don’t hesitate. Say: “I think there’s a mistake.” Most pharmacists will thank you. In fact, 92% of pharmacists say they want patients to verify their prescriptions. But if they brush you off, say: “I’d like to speak to the manager.” If they still won’t listen, walk out. Then call your doctor and report it. You can also report errors to the FDA’s MedWatch program. One man in Ohio reported a pharmacy gave him his wife’s heart medication. He got a call from the FDA a week later saying they’d shut down the pharmacy for repeated violations.
Why This Matters More Than You Think
Verifying your prescription isn’t just a good habit - it’s a lifesaver. Research shows that when patients check their meds, medication errors drop by nearly 37%. That’s not a small number. It means thousands of people avoid hospital visits, ER trips, and even death every year just by taking two minutes to look at their bottle. And it’s not just about pills. It’s about trust. If you don’t verify, you’re letting someone else do your safety check. And that’s a risk no one should take.
What to Do If You’re Over 65 or Have Trouble Reading
If you’re older or have trouble reading small print, you’re not alone. Over 64% of seniors struggle with pharmacy labels. Ask for a magnifying glass - most pharmacies have them. Use your phone’s camera to zoom in. Ask the pharmacist to read the label aloud while you watch. Some pharmacies now offer “verification stations” with tablets that show pictures of the medication. Ask if they have one. You deserve to understand what you’re taking.
Final Tip: Prepare Before You Go
Before you head to the pharmacy, write down:
- The name of the medication
- The dose
- How often to take it
- Why your doctor prescribed it
Bring that list with you. Compare it to the label. If anything doesn’t match, say something. You’re not just a customer. You’re the last line of defense.
What should I do if I realize I took the wrong medication after leaving the pharmacy?
Call your doctor or pharmacist immediately. Don’t wait to see if you feel sick. Even if you feel fine, the wrong medication can cause delayed reactions. If it’s an emergency, call 911 or go to the nearest ER. Bring the bottle with you - even if it’s empty. The pharmacist can check what was supposed to be in it and help determine if you’re at risk.
Can I verify my prescription if I pick it up through mail order or a drive-thru?
Yes - and it’s even more important. Mail-order pharmacies have higher error rates than in-person pharmacies. When your package arrives, open it right away. Compare the label to your doctor’s instructions. Count the pills. Check the expiration date. If something’s off, call the pharmacy before you take any pills. Don’t assume it’s correct just because it came in the mail.
Why do I sometimes get a different-looking pill even though it’s the same medicine?
That’s because of generic drugs. The same medicine can come from different manufacturers, and each one makes the pill look different - different color, shape, or markings. It’s still the same active ingredient. But you need to check the name and strength on the label. If the name and dose match what your doctor prescribed, it’s safe. If you’re unsure, ask the pharmacist to confirm it’s the same medication.
Are pharmacies required to let me check my prescription?
Yes. Under federal guidelines, pharmacists must provide you with counseling and allow you to inspect your medication before you leave. You have the right to ask questions, request a different bottle, or ask to see the original prescription. No pharmacist can legally refuse you this right. If they do, report them to your state’s board of pharmacy.
How often should I verify my prescriptions?
Every single time. Even if you’ve taken the same medication for years. Manufacturers change packaging. Pharmacies switch suppliers. Doses get adjusted. What was safe last month might be wrong this month. Verifying your prescription isn’t a one-time task - it’s a habit. Treat it like checking your seatbelt before driving.
Write a comment
Your email address will not be published.



15 Comments
Just picked up my dad’s blood pressure med yesterday and did the whole checklist. Counted the pills, read the label out loud, checked the expiration. Turns out they gave him 10mg instead of 5mg. Pharmacist apologized and fixed it right away. Honestly? I’m kinda glad I did this. Feels like we’re taught to just trust the system, but nah. We gotta be our own safety net.
It’s frankly astonishing that patients are expected to perform pharmacovigilance duties that should be the purview of licensed professionals. The systemic degradation of pharmacy standards is a direct consequence of cost-cutting measures and regulatory capture. If your pharmacist can’t be trusted to dispense correctly, then the entire healthcare infrastructure is compromised. This isn’t patient empowerment-it’s institutional failure dressed up as a checklist.
my grandma cant read good and she’s scared to ask questions. i started goin with her to the pharmacy and readin everything out loud. she cried the first time she realized she’d been takin the wrong dose for months. we got it fixed. no one should feel too shy to ask. you’re not botherin anyone-you’re savin lives.
There’s an epistemological asymmetry here: the patient possesses incomplete information, yet is expected to validate the output of a system designed to be authoritative. The checklist functions not as a safeguard, but as a compensatory mechanism for institutional incompetence. The real solution isn’t patient vigilance-it’s accountability. When the pharmacist is incentivized to move volume over verification, the burden shifts unfairly. We’re treating symptoms, not causes.
Wow. So now I’m supposed to be a pharmacist too? Next they’ll want me to diagnose my own pneumonia. I work 60 hours a week. I don’t have time to count pills. If the pharmacy screws up, that’s their problem. I’m not a nurse, I’m just trying to get my damn headache meds.
YOU ARE THE LAST LINE OF DEFENSE!! 💪 This is so important!! I used to just grab my meds and run, but now I check EVERYTHING. I even take a pic of the label and compare it to my doctor’s note. You guys, it changed my life. I feel so empowered. Don’t be like me before-I was so careless. Now I’m a medication ninja. 🥷💊
They’re making us check our meds because the government and Big Pharma are hiding something. Why do you think the labels are so small? Why do they use confusing abbreviations? This isn’t about safety-it’s about control. They want you dependent. They want you confused. They want you too tired to fight back. Wake up. This is all part of the plan.
Let me tell you something that nobody else will admit: pharmacies are run by underpaid, overworked people who are one bad day away from giving you your neighbor’s insulin. I’ve seen it. I’ve worked in one. The system is broken. The checklist isn’t optional-it’s survival. And if you think your pharmacist is your friend? They’re just trying to get through their shift without getting sued. Don’t trust them. Verify. Always.
I used to think this was overkill. Then my sister got the wrong antidepressant. She didn’t say anything because she didn’t want to be "difficult." Three days later she was in the hospital. Don’t be like her. Ask questions. Speak up. You’re not being annoying-you’re being brave. And if you’re reading this? You’re already ahead of 90% of people. Keep going.
I’m a pharmacist of 18 years. I’ve seen the worst. I’ve also seen patients who saved their own lives by asking, "Wait, this doesn’t look right." I’m not just saying this-I’m begging you: DO THIS CHECKLIST. I’ve cried after seeing someone catch a mistake because they took two minutes. You’re not a burden. You’re a hero. Thank you for reading this. Seriously. Thank you.
Look, if you can’t read the label, maybe you shouldn’t be taking prescription meds. I mean, come on. This isn’t a parenting blog. If you need someone to read the bottle to you, get a caregiver. Or better yet, don’t be so incompetent that you need a 12-step verification ritual just to take a pill.
in india we just take whatever they give us. no one checks. but then again, we dont have this much paperwork. also, how do you know your doctor didnt mess up? maybe the real problem is doctors not pharmacists. maybe the system is rigged. maybe its all fake.
People are dumb. They don’t check their meds. They get mad when they feel weird. Then they blame the pharmacy. But they didn’t even look at the bottle. It’s not the pharmacy’s fault. It’s yours. You’re lazy. You’re careless. You’re the problem.
Just did this with my mom’s new heart med 💖 I used my phone’s magnifier, read it out loud, and even asked the pharmacist to show me the original script. She smiled and said, "You’re the kind of patient we love." 🤍 You’re not being annoying-you’re being amazing. Keep doing this. The world needs more of you. 💪❤️
It’s fascinating how the article conflates patient vigilance with systemic efficacy. One cannot substitute for the other. The checklist is a Band-Aid on a hemorrhage. True safety requires standardized electronic prescribing, AI-assisted dispensing, and mandatory pharmacist-to-patient audio confirmation protocols. What we’re seeing here is performative safety-a social media-friendly checklist that absolves institutions of responsibility while making patients feel like they’re doing their part. It’s not empowerment. It’s exploitation.