
Breastfeeding Medication Safety Checker
Check if your medication is safe while breastfeeding using the medical community's L1 to L5 risk classification system.
When you're breastfeeding, taking a pill for pain, depression, or an infection isn't just about you. It’s about your baby too. Every time you swallow a medication, a small amount can end up in your breast milk. But here’s the truth most people don’t tell you: breastfeeding medications are almost always safe. Less than 2% of babies show any real side effects from what passes through milk. The fear? It’s often bigger than the risk.
How Medications Get Into Breast Milk
Medications don’t travel to breast milk by magic. They move through your bloodstream, then cross into milk the same way oxygen and nutrients do-mostly by passive diffusion. The bigger the molecule, the harder it is to get through. Drugs under 200 daltons (like ibuprofen or amoxicillin) slip in easily. Larger ones, like heparin or insulin, barely make it at all. Lipid solubility matters too. If a drug loves fat, it’s more likely to enter milk. That’s why some antidepressants and anti-anxiety meds show up in higher amounts. But here’s the twist: just because a drug is in milk doesn’t mean your baby absorbs it. Most babies have immature guts. They don’t absorb much orally, especially if the drug is poorly absorbed or broken down by stomach acid. Protein binding is another gatekeeper. If 90% or more of a drug is stuck to proteins in your blood, it can’t float freely into milk. That’s why drugs like warfarin or phenytoin rarely cause issues. Half-life matters too. A drug that sticks around for 24 hours or more might build up in milk over time. Shorter half-life drugs like acetaminophen clear out fast-so timing your dose helps. In the first few days after birth, your milk is colostrum. It’s thick, low in volume (only 30-60 mL a day), and your breast cells aren’t fully sealed yet. That means more drugs *could* get through. But because so little milk is being consumed, the actual amount your baby gets is tiny. By day five, milk volume increases, but so does the barrier. So even though more milk means more volume, the concentration of drugs often drops.The L1 to L5 Risk System You Can Trust
Dr. Thomas Hale created the most used system for judging medication safety during breastfeeding: L1 to L5. - L1 (Safest): Drugs like acetaminophen, ibuprofen, and penicillin. No reported adverse effects in infants. Used safely for decades. - L2 (Probably Safe): Fluoxetine, sertraline, amoxicillin-clavulanate. Limited data, but no harm shown in large groups of babies. - L3 (Probably Safe with Caution): Some SSRIs, metformin, and certain antibiotics. May cause mild side effects in rare cases-like fussiness or loose stools. Often still recommended because benefits outweigh risks. - L4 (Possibly Hazardous): Lithium, cyclosporine, some chemotherapy drugs. Risk is real. Use only if no alternatives and under close monitoring. - L5 (Contraindicated): Radioactive isotopes, certain cancer drugs, ergotamine. These can cause serious harm. Breastfeeding must stop. You won’t find L5 drugs in your medicine cabinet unless you’re in a hospital. And even then, doctors often find ways to pause treatment or pump and dump temporarily.What Medications Are Most Commonly Used?
Over half of breastfeeding moms take at least one medication. The top three? Pain relievers, antibiotics, and mental health drugs. - Analgesics (28.7%): Ibuprofen and acetaminophen are first-line. They’re in L1. Codeine? Not so much. It turns into morphine in your body, and some moms metabolize it too fast-leading to dangerous levels in milk. Avoid codeine if you can. - Antibiotics (22.3%): Amoxicillin, cephalexin, azithromycin-all L1 or L2. Even metronidazole, once feared, is now considered safe at standard doses. Only avoid if your baby has a known allergy or gets diarrhea that doesn’t clear. - Psychotropics (15.6%): Sertraline and escitalopram are the go-tos for depression and anxiety. They have the lowest transfer rates and least side effects in babies. Fluoxetine? It lingers. It’s L2, but some babies get jittery or have trouble sleeping. Switching to sertraline often helps. You might hear horror stories about SSRIs causing “autism” or “developmental delays.” No study backs that up. The real risk? Not treating your depression. Untreated maternal mental illness harms babies more than any medication ever could.When Timing Matters
You don’t need to pump and dump unless you’re on a drug like L5. But timing your dose can cut your baby’s exposure by half. Take your medication right after you breastfeed. That gives your body time to clear it before the next feeding. For example, if your baby sleeps 6 hours at night, take your pill right after the bedtime feeding. By morning, most of the drug is gone. For drugs taken multiple times a day, like antibiotics, take them just before the feeding with the longest gap. That way, the peak concentration in your milk happens when your baby isn’t nursing. Avoid long-acting or extended-release versions if possible. A quick-release pill taken twice a day is safer than a once-daily slow-release version.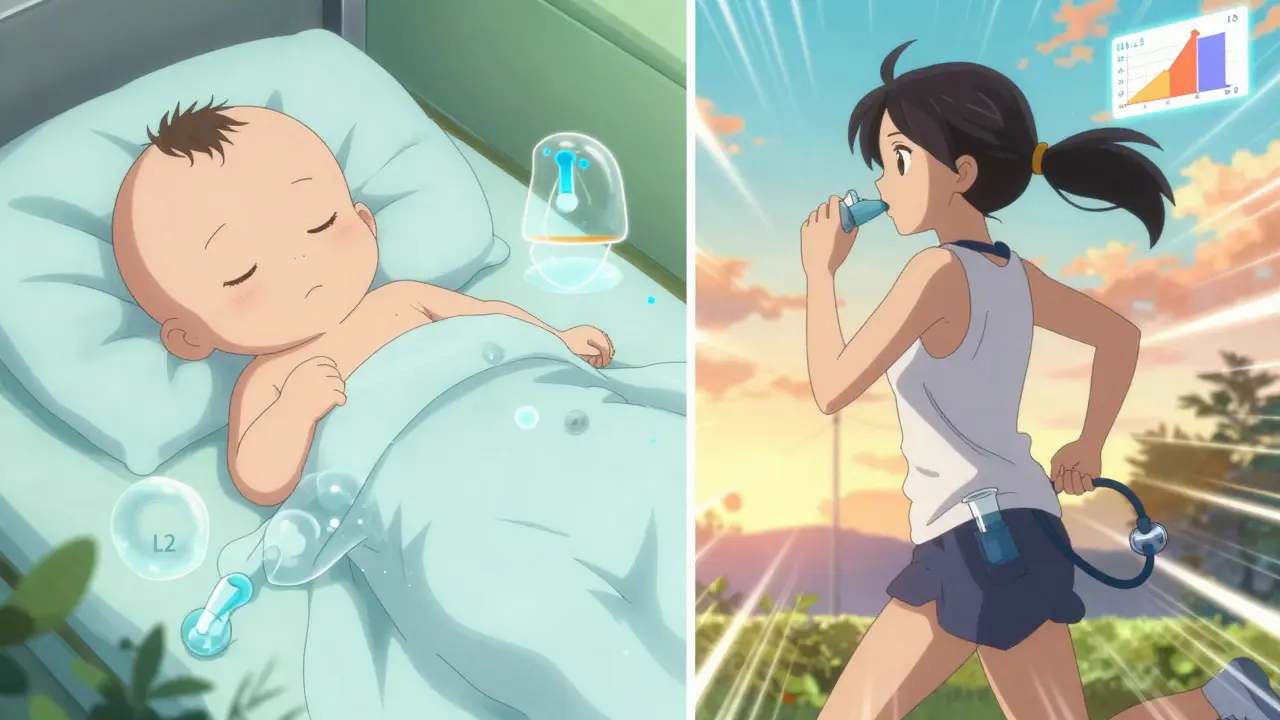
Topical and Inhaled Meds Are Safer
If you’re using a cream, spray, or inhaler, you’re already ahead. Only a tiny amount enters your bloodstream. That means almost nothing reaches your milk. Corticosteroid creams for eczema? Safe. Inhalers for asthma? Safe. Even lidocaine patches? Safe. Just avoid applying creams directly to the nipple before feeding. Wash it off first. The same goes for eye drops and nasal sprays. You’d need to take dozens of doses to get enough into your blood to affect milk.What Resources Should You Use?
Don’t guess. Don’t rely on Google. Use trusted, science-backed tools. - LactMed (from the NIH): Free, updated daily, covers over 4,000 drugs and 350 herbs. It’s technical, but you can search by drug name and get details on infant exposure, half-life, and risk level. Over 1.2 million people use it every year. - Medications and Mothers’ Milk by Dr. Hale: The gold standard. Uses the L1-L5 system. Easier to read than LactMed. Great for quick decisions. - MotherToBaby: A free service run by OTIS. Call or chat with a specialist. They handle 15,000 calls a year. Ask about antidepressants, pain meds, or antibiotics-they’ve seen it all. Most lactation consultants and pediatricians don’t know the details. But these tools? They’re designed for you.What to Watch For in Your Baby
Most babies show no signs at all. But if you’re nervous, look for: - Unusual sleepiness or fussiness - Poor feeding or weight gain - Diarrhea or rash - Jaundice that won’t clear These are rare. But if you notice them, call your doctor. Don’t stop breastfeeding without checking first. Often, switching to a different drug fixes it.What About Herbal Supplements and CBD?
LactMed now includes over 350 herbal products and 200 supplements. But here’s the catch: they’re not regulated. There’s no guarantee of purity, dose, or safety. Chamomile? Probably fine in tea. But high-dose supplements? Unknown. CBD? No reliable data. The FDA warns against it during breastfeeding. Even if it’s “natural,” it can cross into milk. Stick to food. If you want to take something for sleep or anxiety, talk to your doctor first. Don’t self-prescribe.The Big Picture: Breastfeeding Wins
The American Academy of Pediatrics says this clearly: “The benefits of breastfeeding should be weighed against the potential risks of drug exposure.” In almost every case, the benefits win. Breast milk lowers your baby’s risk of infections, allergies, obesity, and sudden infant death. For you, it cuts the risk of breast cancer, ovarian cancer, and type 2 diabetes. If you need a medication, you don’t have to choose between your health and your baby’s. You can have both. The data is clear. The tools are ready. The advice is simple: check LactMed, talk to a specialist, and keep nursing.What’s Coming Next
In 2022, the FDA started pushing drug companies to include breastfeeding women in clinical trials. Right now, only 12 of 85 FDA-approved biologics (like Humira or Enbrel) have any breastfeeding data. That’s changing. The InfantRisk Center’s MilkLab project has already measured drug levels in over 1,250 mothers. Soon, we’ll have personalized predictions-using your genetics to say exactly how much of a drug will end up in your milk. By 2030, doctors may test your DNA before prescribing. If you’re a fast metabolizer of certain drugs, they’ll adjust your dose or choose a different one. No more guessing. No more fear. You’re not alone. You’re not breaking the rules. You’re doing what millions of moms do: taking care of yourself so you can take care of your baby. And that’s not just safe. It’s powerful.Write a comment
Your email address will not be published.




10 Comments
So my cousin took amoxicillin and her baby got a rash-she stopped nursing and cried for days. But now she says maybe she shouldn’t have panicked. This post helped.
Bro, LactMed is the real MVP. I was on sertraline and panicked till I checked it-L2, low transfer, baby chill as hell. Don’t trust your OB’s gut. Go straight to the source. Also, avoid anything with ‘extended release’-it’s just the pharma companies trying to make you suck on a slow drip of chemicals. Go for the quick-release, time it after feed, and boom-you’re a superhero mom.
UK moms don’t even worry about this. We’ve been nursing on antibiotics since the 50s. America overthinks everything.
The data is overwhelming: untreated maternal depression does more damage to infant development than SSRIs ever could. We’ve had decades of longitudinal studies showing this. Yet so many moms still quit nursing because they’re scared of a 0.1% chance of fussiness. The real tragedy isn’t the drug-it’s the silence around mental health. You’re not failing your baby by taking care of yourself. You’re saving them.
What if the FDA is hiding the truth? I read a blog that said all these meds are linked to autism and the WHO is covering it up because Big Pharma owns them. My friend’s cousin’s neighbor’s kid got diagnosed after her mom took ibuprofen. What if this is just the tip of the iceberg? I’m not taking chances. I’m switching to formula. No way I’m risking my baby for a ‘safe’ pill.
YOOOOO I JUST TOOK IBUPROFEN AFTER MY 2AM FEED AND MY BABY DIDN’T EVEN FLINCH. LIKE BRO. YOU CAN DO THIS. DON’T LET FEAR WIN. I’M ON ANTIBIOTICS RIGHT NOW AND MY KID IS STILL SMILING. LACTMED IS YOUR BEST FRIEND. STOP SCROLLING, START CHECKING. YOU GOT THIS.
...And yet, the article conveniently ignores the fact that over 40% of these ‘safe’ drugs have never been tested in neonates under 72 hours old. The L1-L5 system? A marketing tool created by a guy who consulted for drug companies. Where’s the long-term neurodevelopmental data? Where’s the peer-reviewed, double-blind, placebo-controlled studies on infants exposed to sertraline for 12+ months? You’re not giving me data-you’re giving me a pamphlet from a pharmaceutical lobby.
There is a quiet revolution happening here-not in labs or courtrooms, but in the dim glow of nightlights and the hushed rhythm of nursing mothers. We are reclaiming agency over our bodies, our medicine, our milk. To fear the molecule is to misunderstand the miracle: that life, in its most fragile form, is not broken by chemistry, but sustained by it. The breast is not a conduit of poison-it is the original pharmacy. And we, in our exhaustion, our doubt, our trembling hands, are its most faithful pharmacists.
Interesting breakdown, but I’m curious-how does the LactMed database handle drug interactions? Like if someone’s on sertraline and ibuprofen together? Is there data on combined exposure? I’ve seen cases where two L1 drugs together caused unexpected fussiness. Maybe the system needs a ‘L1+’ category for combos.
So let me get this straight-you’re telling me it’s fine to take antidepressants while breastfeeding but I should avoid CBD because it’s ‘not regulated’? What about the 12 million American moms who take melatonin gummies every night? Those aren’t regulated either. And they’re full of sugar and fillers. But hey, if it’s FDA-approved, it’s holy? This whole system is a scam. I’m done trusting anyone who works with a hospital.