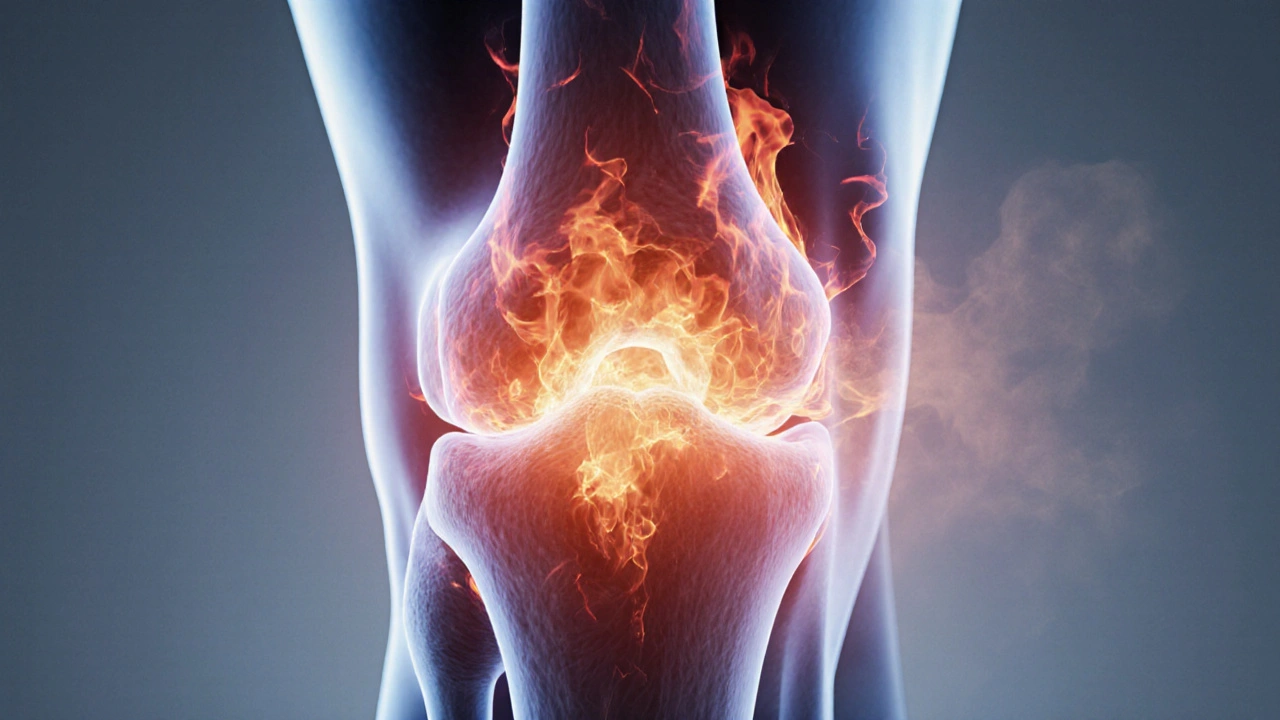
Joint Burning Sensation Symptom Checker
Possible Causes
Recommended Actions
Understanding Joint Burning Sensations
A burning sensation in joints can indicate various conditions including arthritis, gout, neuropathy, or medication side effects. This tool helps identify potential causes based on your symptoms and medical history.
Note: This is for educational purposes only and should not replace professional medical advice.
Quick Takeaways
- Joint burning can signal inflammation, nerve irritation, or metabolic issues.
- Common culprits include arthritis, gout, neuropathy, and medication side‑effects.
- Diagnosis starts with history, physical exam, and a few simple lab tests.
- Treatment mixes medication, lifestyle tweaks, and targeted therapy.
- Early action usually stops the sensation from becoming chronic.
What Is a Burning Sensation in the Joints?
When a joint feels like it’s on fire, tingling, or radiating heat, most people call it a Joint Burning Sensation a painful, heat‑like feeling that occurs in one or more joints, often indicating inflammation, nerve irritation, or metabolic disturbances. It’s different from a dull ache or stiffness; the heat‑like quality often signals that nerves are involved as well as the joint structures themselves.

Why Does It Happen? Common Causes Explained
Below are the most frequent reasons your joints might start to feel like they’re burning. Each cause has its own quirks, but they all end up triggering the same uncomfortable signal.
1. Inflammatory Arthritis
Inflammatory arthritis an autoimmune condition where the body’s immune system attacks joint linings, causing swelling, redness, and a burning pain includes diseases like rheumatoid arthritis and psoriatic arthritis. The immune attack releases cytokines that irritate nerve endings around the joint, creating that hot, stinging feeling.
2. Osteoarthritis (Degenerative Joint Disease)
Osteoarthritis a wear‑and‑tear condition where cartilage thins, bone rubs against bone, and inflammation can flare is usually thought of as a “creaky” joint, but when cartilage breaks down, tiny bone fragments can irritate nearby nerves, resulting in a burning sensation especially after activity.
3. Gout
Gout a crystal‑induced arthritis caused by excess uric acid depositing sharp needles in joints, most often the big toe can erupt suddenly with excruciating heat and throbbing. The crystal inflammation awakens pain fibers, giving that classic “burning” feeling.
4. Peripheral Neuropathy
Peripheral neuropathy damage to peripheral nerves that often produces tingling, burning, or shooting pains in extremities isn’t a joint disease per se, but nerves that run close to joints can become over‑reactive. Diabetes, alcohol misuse, and certain chemotherapies are top triggers.
5. Raynaud’s Phenomenon
Raynaud’s phenomenon a vascular disorder where small arteries spasm, limiting blood flow and causing cold‑induced burning sensations usually hits fingers and toes, but when joints are involved the reduced circulation can create a prickly, hot feeling once blood returns.
6. Medication Side‑Effects
Some drugs, especially certain cholesterol‑lowering statins, fluoroquinolone antibiotics, and chemotherapy agents, list joint pain as a side‑effect that may include burning, tingling, or stiffness. The exact mechanism varies, but many interfere with mitochondrial energy in nerves.
7. Infections
Joint infections like septic arthritis or Lyme disease can cause intense inflammation that feels like burning. Even a mild viral infection (e.g., parvovirus) may provoke a temporary joint‑burning episode.
How to Pinpoint the Culprit - Diagnosis Steps
- Medical History: Note when the burning started, which joints are affected, any recent injuries, new meds, diet changes, or illnesses.
- Physical Examination: A clinician will look for swelling, warmth, limited motion, and check for nerve‑related signs like altered sensation.
- Blood Tests: Common panels include complete blood count, C‑reactive protein (CRP), erythrocyte sedimentation rate (ESR), uric acid, and fasting glucose to screen for inflammation, gout, and diabetes‑related neuropathy.
- Imaging: X‑rays reveal bone erosions (arthritis) or joint space narrowing (osteoarthritis). Ultrasound can catch early inflammation, while MRI helps see soft‑tissue and nerve involvement.
- Joint Fluid Analysis: If infection or gout is suspected, a doctor may aspirate fluid to look for crystals or bacteria.
- Nerve Studies: Electromyography (EMG) or nerve conduction tests confirm peripheral neuropathy when pain outpaces joint findings.
Getting the right diagnosis is crucial because the treatment path changes dramatically between an autoimmune flare and a medication side‑effect.
Treatment Options - From Quick Relief to Long‑Term Management
Below is a toolbox of strategies. Most patients need a mix, not a single magic bullet.
Medication‑Based Relief
- Non‑steroidal anti‑inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, reduce inflammation and can blunt the burning feeling - good first‑line for arthritis or gout.
- Corticosteroids oral or injectable steroids that rapidly suppress immune‑driven inflammation - reserved for severe flares or when NSAIDs aren’t enough.
- Disease‑modifying antirheumatic drugs (DMARDs) such as methotrexate or sulfasalazine, used for inflammatory arthritis to prevent joint damage.
- Uric‑lowering therapy allopurinol or febuxostat, long‑term meds that keep uric acid low and stop gout attacks.
- Neuropathic pain agents like gabapentin or duloxetine, which calm over‑active nerves causing burning sensations.
Physical Therapy & Rehabilitation
Physical therapy a structured program of targeted exercises, manual techniques, and modalities to improve joint mobility and reduce nerve irritation can be a game‑changer. Gentle range‑of‑motion work, strengthening of surrounding muscles, and heat‑/cold therapy together lower the “fire” feeling.
Lifestyle Tweaks
- Weight Management: Carrying extra pounds adds stress to weight‑bearing joints (knees, hips). Losing even 5‑10% of body weight can cut inflammation dramatically.
- Diet: Foods rich in omega‑3 fatty acids (salmon, chia seeds) and antioxidants (berries, leafy greens) help calm systemic inflammation. Limiting high‑purine foods (red meat, shellfish) benefits gout patients.
- Hydration: Adequate water helps kidneys flush uric acid and keeps joint cartilage lubricated.
- Ergonomic Adjustments: Using proper keyboards, supportive shoes, and correct lifting techniques prevents joint strain that can trigger burning sensations.
Complementary Therapies
- Acupuncture: Small needles placed near the joint can modulate pain pathways, offering relief for some people with neuropathic joint pain.
- Topical Capsaicin: Derived from chili peppers, it depletes substance P-a neurotransmitter involved in burning pain-when applied regularly.
- Mind‑Body Practices: Yoga, tai chi, and guided breathing lower stress hormones that can amplify inflammatory responses.

Prevention - Keeping the Burn at Bay
Even if you’ve never felt that scorching joint pain, adopting these habits lowers your risk.
- Stay active with low‑impact cardio (swimming, cycling) to keep synovial fluid flowing.
- Schedule annual check‑ups for blood sugar and cholesterol; early control prevents nerve damage and gout.
- Rotate repetitive motions-if you work at a desk, stand up every hour and stretch.
- Know your meds: ask your pharmacist if a new prescription lists joint pain as a side‑effect.
Comparison Table - Common Causes vs Typical Treatments
| Cause | Key Treatment(s) | Typical Onset of Relief |
|---|---|---|
| Inflammatory arthritis | DMARDs, NSAIDs, physical therapy | 2-4 weeks (DMARDs may take longer) |
| Osteoarthritis | Weight loss, NSAIDs, targeted exercise | Days to weeks |
| Gout | NSAIDs, colchicine, uric‑lowering meds | Hours to days (colchicine works fast) |
| Peripheral neuropathy | Gabapentin, lifestyle control of diabetes/alcohol | 1-2 weeks |
| Medication side‑effects | Switch drug, symptomatic NSAIDs, dose adjustment | Days after change |
| Raynaud’s phenomenon | Warm clothing, calcium channel blockers, biofeedback | Weeks for medication effect |
Frequently Asked Questions
What does a burning sensation in the joints feel like?
It usually feels like heat or a mild flame inside the joint, often accompanied by tingling, pins‑and‑needles, or a sharp sting that worsens with movement.
Can gout cause a burning sensation, or is it just throbbing pain?
Gout crystals trigger intense inflammation, and many patients describe the pain as burning or hot. The sensation often peaks within 24hours of an attack.
Are NSAIDs safe for long‑term use to treat joint burning?
Occasional NSAID use is fine, but chronic daily use can upset the stomach, affect kidneys, and raise cardiovascular risk. Talk to a doctor about the safest schedule or alternatives.
How quickly can physical therapy relieve joint burning?
Most people notice reduced heat and stiffness after 2‑3 sessions when the therapist focuses on gentle mobilization and muscle strengthening. Consistency over 4‑6 weeks yields the best results.
Is burning sensation ever a sign of something serious like infection?
Yes. Septic arthritis can cause sudden, intense heat, swelling, and fever. If you have fever, rapidly worsening pain, or redness, seek medical care right away.
If you’ve been dealing with that unsettling heat in your joints, you now have a roadmap: figure out the cause, get the right tests, and apply a mix of meds, movement, and lifestyle tweaks. Most people see relief within a few weeks when the treatment matches the underlying issue. Don’t let the burn linger-address it early, and you’ll keep your joints comfortable for the long haul.
Write a comment
Your email address will not be published.




14 Comments
Reading through that exhaustive breakdown makes me think of the body as a tiny philosophical battlefield – nerves firing like arguments, inflammation marching like troops. When the joint feels like it’s on fire, it’s really a signal that some deeper discourse is happening inside our tissues. The key is to listen, not just to the heat, but to the context: diet, stress, genetics. Treating the symptom without understanding the cause is like debating without knowing the premise.
Wow this is drama central a burning joint is like a volcano ready to explode and you just read the whole textbook lol
Hey folks, love how this post paints a bright picture of hope even when your joints feel like they’re auditioning for a fireworks show! 🌈 Remember, every spark of pain is a chance to shine a light on lifestyle tweaks – sip more water, toss those sugary snacks, and let those omega‑3s do their magic. You’ve got the tools, so fire up that optimism and give those joints a gentle hug.
I feel you on the heat in the joints – it can be unsettling. It helps to keep a symptom diary to spot patterns and share them with a doctor. Small changes like staying hydrated and gentle stretching often bring relief.
Okay let me just pour it all out in simple terms because sometimes the medical jargon feels like a wall of noise and I need to break it down for real people like us 😅 so first thing you know when a joint feels like it’s on fire is that there’s likely some irritation either from inflammation or nerve signals and that can come from a bunch of stuff like gout arthritis or even a side effect from meds the good news is that most of these have clear steps you can take for relief you can start with basic home care like resting the joint applying a cool pack or a warm compress depending on what feels better and then move on to over the counter NSAIDs if you’re not allergic and they don’t bother your stomach also consider your diet cutting back on high purine foods if gout is a suspect and staying hydrated helps your kidneys flush out excess uric acid remember that lifestyle tweaks like losing a few pounds if you’re carrying extra weight can reduce stress on weight‑bearing joints and regular low‑impact exercise keeps the synovial fluid moving what’s more if you suspect a nerve issue like peripheral neuropathy managing blood sugar is key and sometimes doctors prescribe gabapentin for that burning nerve pain finally keep a log of what you try and how you feel so you can show a health professional a clear picture of what works and what doesn’t 😊
If you’re looking for a concise action plan, start with the basics: 1) Rest the affected joint and avoid activities that aggravate it. 2) Apply ice for 15‑20 minutes several times a day if there’s swelling, or heat if stiffness dominates. 3) Over‑the‑counter NSAIDs such as ibuprofen can reduce inflammation, but take them with food to protect your stomach. 4) Schedule a visit with your primary care provider for blood work – they’ll check CRP, ESR, uric acid and glucose to narrow down the cause. 5) Follow up with a specialist (rheumatologist or neurologist) based on those results. This stepwise approach covers most common triggers without overwhelming you.
Stop ignoring the burn – get checked now, you’re not going to fix this with wishful thinking.
Hey buddy look i know this sounds like a lecture but trust me it's important – if you keep pushing through the heat you might end up with bigger problems later 🤝 so take a step back, hydrate, and maybe get a doc to run some labs. Also try not to overdo the meds, sometimes they can backfire. Stay safe and keep an open mind – we all learn together.
Overall, the article does a solid job of summarizing causes, diagnostics, and treatment options. It’s a good starting point for anyone experiencing joint burning sensations.
Oh sure, because the government’s secret plan to hide the truth about joint pain is totally a thing. If you read the article you’ll spot the hidden code that says “Take pills, ignore your gut feelings.” Classic.
Don’t get discouraged – even a tiny step towards healthier habits can dim that burning feeling. You’ve got this, keep moving forward!
Interesting read – as if we didn’t already know our joints could feel like tiny furnaces. Thanks for the reminder.
Let us, for a moment, plunge into the abyss of existential ache that a burning joint represents, for it is not merely a physiological event but a metaphor for the human condition itself. The fire licking the cartilage whispers of a world where entropy reigns, where the body, that fragile vessel, rebels against its own temporality. In this grand theater, the inflammatory cascade is akin to a chorus of dissenting voices, each cytokine a soliloquy of sorrow, each prostaglandin a lament for lost equilibrium. One might argue that the sensation of heat is the body’s own Sisyphean attempt to illuminate the hidden fissures of neglect, diet, and stress that have accumulated like dust on an ancient tome. To address this, we must first acknowledge that medicine, though a marvel, is but a bandage on the deeper scar of lifestyle. A balanced diet, rich in anti‑inflammatory omega‑3s, becomes a poet’s ode to cellular harmony, while regular movement – the graceful dance of low‑impact exercise – serves as a dialogue between muscle and joint, coaxing the synovial fluid into a harmonious rhythm.
Consider, too, the role of the mind: chronic stress, that invisible tyrant, releases cortisol, which in turn fans the flames of inflammation. Meditation, mindful breathing, and even a simple walk in nature can act as a cool breeze, tempering the blaze. When pharmacology enters the scene – NSAIDs, colchicine, DMARDs – they perform as supporting actors, providing temporary relief, yet they cannot replace the leading role of prevention.
Thus, the burning joint is both a symptom and a summons. It calls upon us to interrogate our habits, to seek balance, and to remember that the body, like a well‑written novel, thrives on consistency, patience, and the occasional plot twist of self‑care. In embracing this holistic narrative, the fire may dim, leaving behind only the gentle warmth of a life lived with intention.
Take it easy, listen to your body, and keep moving forward one step at a time.