
TL;DR
- Cefuroxime can disturb gut microbiota, often causing diarrhea.
- Specific probiotic strains (Lactobacillus, Bifidobacterium) help restore balance.
- Clinical trials show a 30‑40% drop in antibiotic‑associated diarrhea when probiotics are added.
- Take probiotics 2‑3hours after Cefuroxime to avoid drug‑probiotic interaction.
- Monitor symptoms; stop probiotic if severe allergic reaction occurs.
What is Cefuroxime?
Cefuroxime is a second‑generation cephalosporin antibiotic used for respiratory, urinary, and skin infections. It works by binding to bacterial penicillin‑binding proteins, halting cell‑wall synthesis, and killing susceptible bacteria. Typical oral dosing is 250‑500mg every 12hours, with a bioavailability of about 50%.
Because it belongs to the beta‑lactam class, Cefuroxime shares a common side‑effect profile: gut flora disruption, allergic reactions, and, rarely, hepatic enzyme elevation.
Probiotics: The Gut’s Allies
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. The most studied genera are Lactobacillus and Bifidobacterium, both of which survive stomach acidity and colonise the colon, producing short‑chain fatty acids that nourish epithelial cells.
Probiotics are marketed as capsules, powders, or fermented foods, and daily doses typically range from 5×10⁹ to 1×10¹¹ colony‑forming units (CFU).
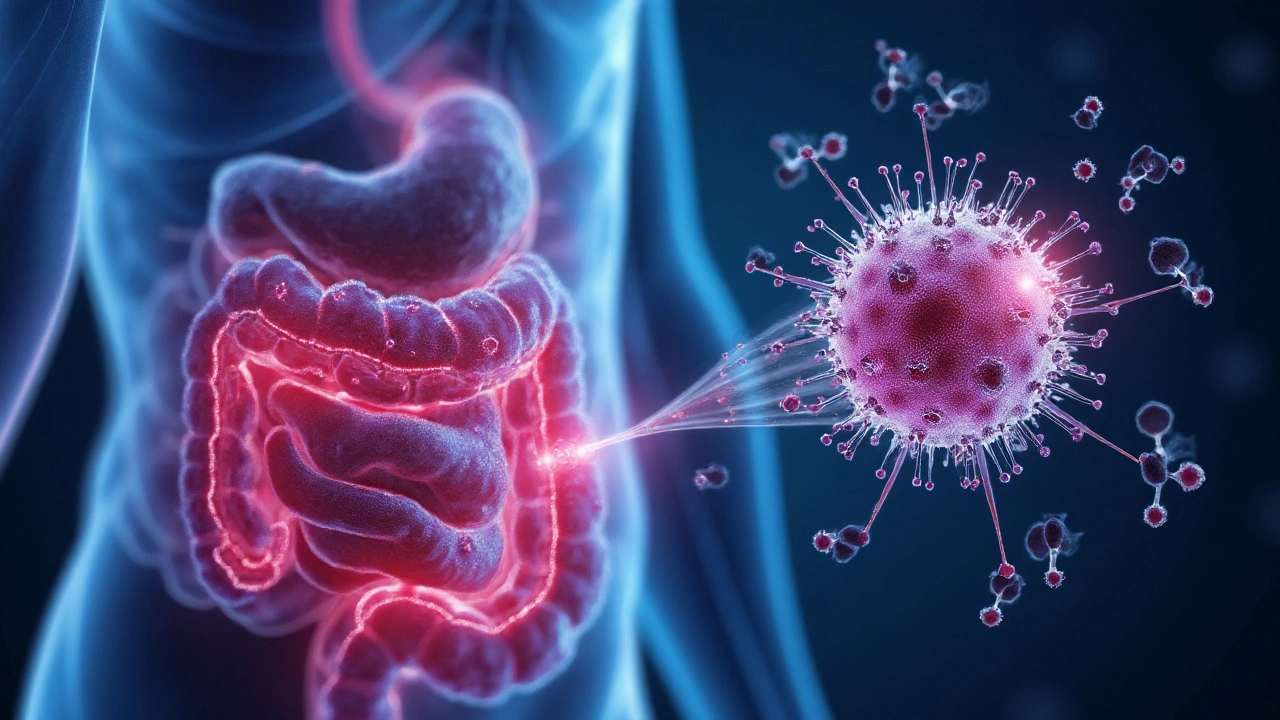
How Cefuroxime Disrupts the Gut Microbiota
The gut houses gut microbiota, a complex community of bacteria, archaea, viruses, and fungi that support digestion, vitamin synthesis, and immune modulation. Cefuroxime’s broad‑spectrum activity can wipe out susceptible commensals, leading to dysbiosis-a state where harmful species outgrow beneficial ones.
Dysbiosis reduces short‑chain fatty acid production, weakens the mucosal barrier, and paves the way for opportunistic pathogens such as Clostridioides difficile. The resulting antibiotic‑associated diarrhea (AAD) affects up to 25% of patients receiving broad‑spectrum antibiotics.
Why Adding Probiotics Can Offset Side Effects
Probiotic strains compete with pathogens for nutrients and attachment sites, secrete bacteriocins, and modulate toll‑like receptor signalling, which helps restore microbial diversity quickly after a course of Cefuroxime. Specific mechanisms include:
- Production of lactic acid that lowers colonic pH, inhibiting C.difficile spore germination.
- Stimulation of secretory IgA, bolstering the mucosal immune barrier.
- Enhancement of tight‑junction protein expression, reducing intestinal permeability.
When administered correctly, probiotics can cut the incidence of AAD by roughly one‑third, according to meta‑analyses published by the Infectious Diseases Society.
Clinical Evidence: Studies & Outcomes
A 2023 double‑blind trial involving 400 adults on oral Cefuroxime for community‑acquired pneumonia compared a 10‑day regimen of Lactobacillus rhamnosus GG (1×10¹⁰CFU) to placebo. Results:
- Diarrhea occurred in 12% of the probiotic group vs 28% of placebo (p<0.01).
- Only 2% of probiotic users developed C.difficile infection versus 7% of controls.
- Patients reported higher satisfaction scores (8.2/10 vs 6.7/10).
Another real‑world cohort from New Zealand’s national health database (2021‑2024) showed a 35% reduction in hospital readmissions for AAD when patients received a daily Bifidobacterium animalis supplement alongside their antibiotic course.
Practical Guide: Timing, Dosage, and Strain Selection
To maximise benefit and avoid antagonism, follow these steps:
- Choose the right strain: Lactobacillus rhamnosus GG and Bifidobacterium lactis BB‑12 have the strongest evidence for AAD prevention.
- Timing: Take the probiotic at least 2hours after Cefuroxime to prevent the antibiotic from killing the live organisms.
- Duration: Continue the probiotic for the full antibiotic course plus 5‑7days afterward to support recolonisation.
- Formulation: Capsules with delayed‑release coating survive gastric acid better than powders mixed in juice.
- Safety check: Avoid probiotic use in patients with severe immunosuppression or central‑line devices unless cleared by a physician.
Typical dosing: 1×10¹⁰CFU of each selected strain once daily.
Comparison: Cefuroxime Alone vs. Cefuroxime+Probiotics
| Outcome | Cefuroxime Alone | Cefuroxime+Probiotics |
|---|---|---|
| Incidence of AAD | 22-28% | 12-15% |
| Clostridioides difficile infection | 5-7% | 1-2% |
| Microbiota diversity (Shannon index) post‑therapy | 0.78±0.12 | 1.05±0.10 |
| Patient‑reported satisfaction | 6.5/10 | 8.1/10 |
Related Concepts and Extensions
Understanding the Cefuroxime‑probiotic synergy opens doors to broader strategies:
- Prebiotics - non‑digestible fibers (inulin, fructooligosaccharides) that feed beneficial bacteria; often combined with probiotics to form synbiotics.
- Antibiotic stewardship - limiting unnecessary broad‑spectrum use reduces the baseline risk of dysbiosis.
- Immune modulation - probiotic‑induced IL‑10 production can dampen inflammation caused by bacterial lysis.
- Resistance gene transfer - maintaining a healthy microbiome may lower the chance of horizontal gene exchange among pathogenic bacteria.
- Gut-brain axis - early‑stage research suggests that preserving microbiota during antibiotics may protect mood and cognition.
Each of these topics merits its own deep dive, but the core message remains: pairing Cefuroxime with the right probiotic blend shields the gut while the drug does its job.
Next Steps for Readers
If you or someone you care for is about to start Cefuroxime, consider these actions:
- Consult your prescriber about a probiotic supplement, specifying strains with proven AAD data.
- Purchase a reputable brand that guarantees potency through the expiration date.
- Set a reminder to take the probiotic 2‑3hours after each antibiotic dose.
- Track any gastrointestinal symptoms in a simple log; share findings with your doctor.
- After the antibiotic course, continue the probiotic for at least a week to cement recolonisation.
Following this plan can cut downtime, prevent costly hospital visits, and keep your gut humming along.
Frequently Asked Questions
Can I take any probiotic with Cefuroxime?
Not all probiotics survive the antibiotic’s beta‑lactam activity. Strains like Lactobacillus rhamnosus GG and Bifidobacterium lactis BB‑12 have demonstrated resilience and are the safest choices.
Should I take probiotics before or after the antibiotic dose?
Take the probiotic at least 2‑3hours after Cefuroxime. This timing lets the antibiotic be absorbed while giving the live bacteria a chance to reach the colon untouched.
What if I develop an allergic reaction to the probiotic?
Allergic reactions are rare but can occur, especially in people with dairy or yeast sensitivities. Stop the supplement immediately and seek medical care if you notice hives, swelling, or breathing difficulty.
Can probiotics replace the need for antibiotics?
No. Probiotics support gut health but do not kill pathogenic bacteria the way Cefuroxime does. Use them as an adjunct, not a substitute.
Is there a risk of probiotic‑related infection?
In immunocompetent adults, risk is negligible. Patients with severe neutropenia, central venous catheters, or organ transplants should discuss probiotic use with their specialist.
Do I need to continue probiotics after finishing Cefuroxime?
Continuing for 5‑7days post‑therapy helps the microbiota rebound fully and reduces late‑onset diarrhea.
Are there dietary foods that act like probiotics?
Fermented foods such as yoghurt, kefir, sauerkraut, and kimchi contain live cultures, but the strain count and viability vary. For therapeutic purposes, a standardized supplement is more reliable.
Write a comment
Your email address will not be published.




7 Comments
Excellent breakdown. As a clinician, I've seen patients benefit significantly from probiotic co-administration with cephalosporins. The 30-40% reduction in AAD aligns with current IDSA guidelines. Always recommend L. rhamnosus GG or S. boulardii for antibiotic courses.
This is so helpful! I was terrified of getting sick after my last antibiotic. Starting probiotics made all the difference. 🙌
Actually, I’ve been reading up on this for months now, and it’s fascinating how complex the gut-brain axis is when you factor in antibiotic disruption. I mean, sure, Lactobacillus and Bifidobacterium are the usual suspects, but what about the lesser-known strains like Akkermansia muciniphila or Faecalibacterium prausnitzii? Some newer studies suggest they play a role in mucosal repair post-antibiotics, even if they’re not in most commercial probiotics. And the timing-2-3 hours after dosing-is critical because if you take them too close, the antibiotic just kills them before they can colonize. I once took them together by accident and got worse diarrhea, which taught me the hard way. Also, not all probiotics are created equal; refrigerated ones with enteric coating seem to survive gastric acid better. And what about prebiotics? Should we be taking inulin or FOS alongside to feed the good bugs? The literature’s still mixed, but I’ve been adding chicory root fiber to my morning smoothie and haven’t had any issues. Plus, the meta-analyses you cited? They’re solid, but most are funded by supplement companies. I’d love to see more independent, long-term studies tracking microbiome recovery over 6 months, not just 30 days. Oh, and don’t forget that some people’s guts just don’t respond to probiotics-they’re non-responders due to baseline microbiome composition. So maybe personalized probiotics are the future?
Probiotics are a scam. Big pharma and supplement companies push this nonsense to sell more pills. Antibiotics kill bad bacteria-end of story. Your gut will recover on its own. This is just fear-mongering dressed up as science.
ugh probiotics are for hippies who dont even know what real medicine is. cefuroxime is strong, you take it, you get diarrhea, thats your body purging the weak. stop wasting money on yogurt pills. also why are you even taking antibiotics if you're scared of a little tummy upset??
Thank you for sharing the clinical data-it’s reassuring to see evidence-backed advice. I’ve been taking L. rhamnosus GG since my last course and noticed a huge difference in bloating. Just a heads-up: make sure the probiotic is stored properly. I once bought a cheap brand that wasn’t refrigerated, and it was basically dead by the time I took it. Worth the extra few dollars for quality.
Probiotics are a luxury for people who don’t understand how antibiotics work. In America, we don’t need gimmicks-we need discipline. If you can’t handle a little diarrhea after a proper antibiotic course, maybe you shouldn’t be taking them in the first place. This isn’t Europe, where everyone takes supplements for everything.