What if the medicine you’re taking to control your high blood pressure is secretly making your asthma worse? Or what if the pill you take for depression is hiding the warning signs of low blood sugar - signs that could save your life? This isn’t hypothetical. Every day, millions of people are caught in hidden dangers called drug-disease interactions - when a medication meant to help one condition accidentally harms another.
What Exactly Are Drug-Disease Interactions?
Drug-disease interactions (also called drug-condition interactions) happen when a drug used to treat one health problem makes another existing condition worse. It’s not about two drugs clashing - that’s a drug-drug interaction. This is about your body’s existing illness reacting badly to a medicine. For example:- Beta-blockers like propranolol help lower blood pressure and reduce heart strain - but they can tighten airways in people with asthma, triggering attacks.
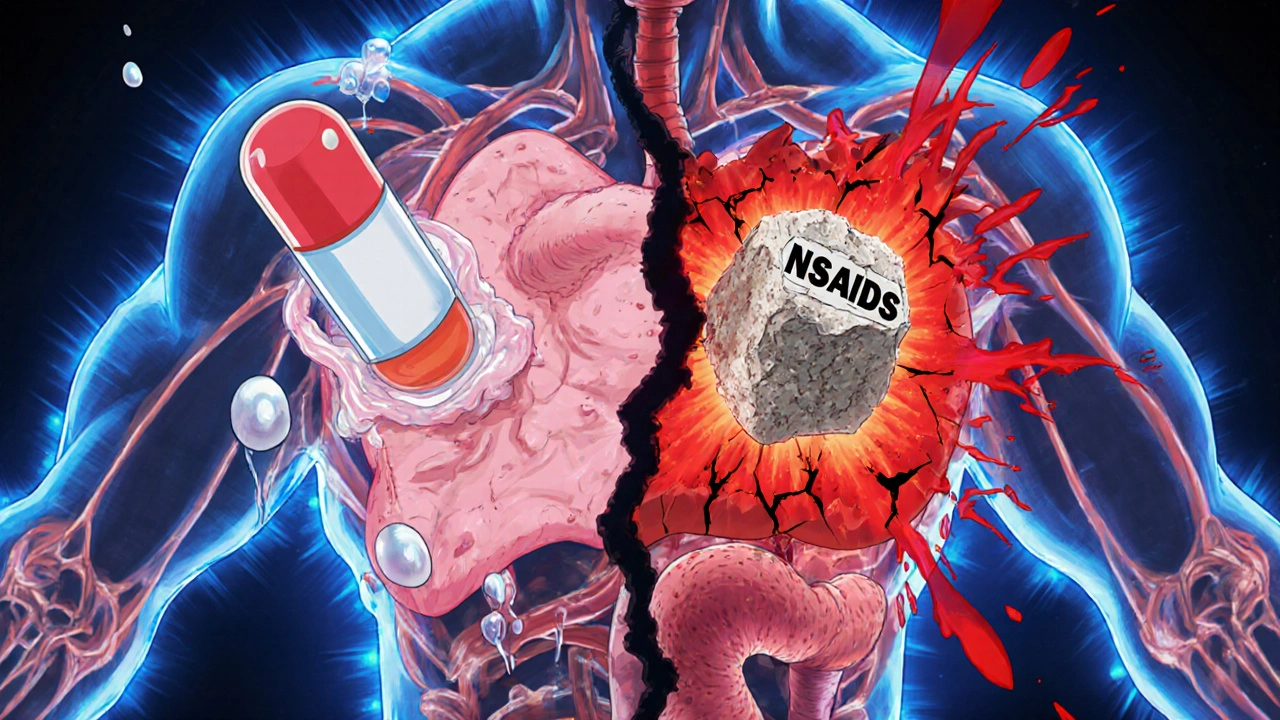
- NSAIDs like ibuprofen reduce pain and swelling, but they cause fluid retention that can push heart failure patients into hospital.
- Metformin, a common diabetes drug, is safe for most - but in someone with kidney disease, it can build up and cause dangerous lactic acidosis.
- SSRIs for depression can increase bleeding risk, especially if you’re also on blood thinners or have ulcers.
How Do These Interactions Actually Happen?
There are five main ways a drug can turn harmful because of your health condition:- Pharmacodynamic interference: The drug’s effect directly fights your disease. Beta-blockers reduce heart rate - great for hypertension - but they also block the body’s natural adrenaline response to low blood sugar. That means someone with diabetes might not feel shaky, sweaty, or hungry when their sugar drops. No warning. No time to act.
- Pharmacokinetic changes: Your disease alters how your body handles the drug. Liver disease slows down how fast your body breaks down warfarin. That means even a normal dose can become toxic, causing internal bleeding.
- Masking symptoms: The drug hides the signs of a problem. Diuretics for heart failure can make you pee more, which might mask worsening kidney function. You think you’re improving - but your kidneys are failing silently.
- Exacerbating complications: The drug worsens the side effects of your condition. NSAIDs cause sodium and water retention. For someone with heart failure, that means more swelling, more shortness of breath, more strain on the heart.
- Direct organ toxicity: The drug poisons an organ already weakened by disease. Lithium for bipolar disorder is cleared by the kidneys. If kidney function drops, lithium builds up - leading to tremors, confusion, seizures, even death.
Who’s Most at Risk?
The biggest risk group? Older adults. The average person over 65 has 4.7 chronic conditions and takes 5.4 medications daily. That’s a recipe for hidden clashes. But it’s not just age. People with these conditions face the highest risk:- Chronic kidney disease: 80% of drugs are cleared through the kidneys. When they’re damaged, drugs pile up. Metformin, lithium, NSAIDs, certain antibiotics - all become dangerous.
- Heart failure: Fluid balance is delicate. NSAIDs, some anti-inflammatories, and even certain diabetes drugs can tip the scales.
- Liver disease: The liver metabolizes most drugs. If it’s scarred or inflamed, drugs stick around too long. Warfarin, benzodiazepines, statins - all need lower doses.
- Diabetes: Many drugs mask hypoglycemia. Beta-blockers, ACE inhibitors, and even some antibiotics can hide the symptoms of low blood sugar.
- Psychiatric conditions: SSRIs and SNRIs increase bleeding risk. Lithium and antipsychotics can be deadly if kidney or thyroid function is off.
Why Do Doctors Miss These?
You’d think this would be easy to catch. But here’s the problem: most clinical guidelines don’t talk about it. A 2015 study found that only 16% of guidelines for diabetes, depression, and heart failure included warnings about drug-disease interactions. That means doctors are following rules that don’t warn them about the biggest dangers. Electronic health records (EHRs) are supposed to help. Epic’s system flags 87% of high-risk interactions - but 42% of those are false alarms. Doctors start ignoring them. Alert fatigue. It’s real. And when you’re rushing between patients, you click past the warning. Community pharmacists spend nearly 13 minutes per patient just checking for these interactions. But in a busy pharmacy, that’s often not possible. Only 32% of patients with high blood pressure even know why decongestants like pseudoephedrine are dangerous - even though they’ve been prescribed them.How to Protect Yourself
You can’t rely on the system to catch everything. Here’s what you can do:- Keep a complete list: Write down every pill, supplement, and OTC drug you take - including doses and why you take them. Bring it to every appointment.
- Ask the three questions:
- Is this drug safe with my other conditions?
- Could it hide symptoms of another problem?
- Will my kidneys or liver handle this?
- Know your numbers: If you have kidney disease, heart failure, or liver issues, know your latest lab values. Ask your doctor what levels are safe for your medications.
- Use the Beers Criteria: This is the gold standard for older adults. It lists drugs to avoid with certain conditions. Ask if your meds are on it.
- Check supplements: Just because it’s “natural” doesn’t mean it’s safe. St. John’s wort, ginkgo, garlic, and ginseng all interact dangerously with common drugs.
- Get a medication review: Ask for a full review with your pharmacist or a geriatric specialist - especially if you take five or more drugs.
What’s Changing in 2025?
The tide is turning. The FDA now requires drug makers to test new medications in patients with common comorbidities - not just healthy volunteers. The European Medicines Agency requires a full drug-disease interaction section in every new drug application. The NIH’s All of Us program is linking genetic data with health records to predict individual risks - early results show 38% better accuracy than old methods. And machine learning? A 2023 study from the University of Toronto showed AI can predict high-risk interactions with 89% accuracy by analyzing 157 clinical factors - far better than old rule-based systems. But here’s the catch: these tools aren’t in most clinics yet. And medical schools still spend less than five hours teaching this topic - even though it’s one of the leading causes of preventable hospital admissions.The Bottom Line
Drug-disease interactions are silent killers. They don’t make headlines. They don’t come with warning labels. But they’re responsible for 5-10% of all hospital admissions - and many of them are preventable. If you’re managing more than one health condition, you’re not just taking medicine. You’re navigating a minefield. The only way out is awareness. Ask questions. Know your conditions. Know your drugs. And never assume a medication is safe just because your doctor prescribed it. Your health isn’t one condition. It’s a system. And every drug you take affects the whole system - not just the one you’re trying to fix.Can a drug that’s safe for most people be dangerous for me?
Yes. A drug that’s perfectly safe for someone with one condition can be harmful if you have another. For example, metformin is a first-line diabetes drug - but if you have kidney disease, it can cause lactic acidosis. Beta-blockers help with high blood pressure but can make asthma worse or hide low blood sugar symptoms. What’s safe for one person isn’t safe for everyone.
Are over-the-counter drugs and supplements risky too?
Absolutely. NSAIDs like ibuprofen can worsen heart failure and kidney disease. Decongestants like pseudoephedrine can spike blood pressure. Even natural supplements like St. John’s wort can trigger serotonin syndrome when mixed with antidepressants. Many people don’t realize OTC meds and herbs are drugs too - and they carry the same risks.
Why don’t doctors always warn me about these interactions?
Many clinical guidelines don’t include drug-disease interaction warnings - only about 16% do. Doctors rely on those guidelines, and electronic systems flood them with false alerts, leading to alert fatigue. Plus, time is tight. A typical doctor visit lasts 15 minutes. Checking for hidden risks across multiple conditions isn’t always possible without a full medication review.
How do I know if my kidneys or liver can handle my meds?
Ask for your latest lab results - especially creatinine, eGFR (for kidneys), and liver enzymes like ALT and AST. If your eGFR is below 60, many drugs need dose adjustments. If your liver enzymes are high, some medications may be unsafe. Your pharmacist can help interpret these numbers in context with your prescriptions.
What should I do if I think a drug is making my other condition worse?
Don’t stop taking it suddenly. Write down what changed - new symptoms, timing, dose. Bring your complete medication list to your doctor or pharmacist. Ask: “Could this drug be affecting my other condition?” They may adjust the dose, switch to a safer alternative, or add monitoring. Your input matters - you’re the expert on how your body feels.
Are there tools or apps that can help me track these risks?
Yes. Apps like Medscape, Epocrates, and Micromedex have drug interaction checkers - but make sure they include disease interactions, not just drug-drug. The Beers Criteria app is free and specifically for older adults. The best tool, though, is a printed, up-to-date list of all your meds and conditions - bring it to every appointment. Technology helps, but human communication saves lives.
Next Steps for Patients
Start today. Take out your pill bottle or phone app. List every medication and supplement. Next to each, write down the condition it’s for. Then ask yourself: “Could this make any of my other conditions worse?” Schedule a medication review with your pharmacist. Ask your doctor if your prescriptions align with the latest Beers Criteria. If you’re on five or more drugs, ask if you can be referred to a geriatric pharmacist or a medication therapy management program. You’re not being paranoid. You’re being smart. Because in the world of multiple conditions and multiple drugs, the safest choice isn’t always the one your doctor prescribes - it’s the one you understand.Write a comment
Your email address will not be published.



15 Comments
Wow. I just read this and sat there for ten minutes, just... thinking. It’s like our bodies are these intricate, whispering machines-each organ humming its own tune, and then some doctor hands you a pill like it’s a magic wand that only plays one note. But no-it’s more like tossing a rock into a pond and watching ripples crash into every other ripple you didn’t even know existed. Beta-blockers hiding low blood sugar? That’s not just a side effect-that’s a silent thief in the night. And we’re all just walking around with our own personal minefields, unaware that the shoe we’re wearing might be the one that triggers it. I mean, who even teaches us this stuff? Not med school, apparently. Not the FDA, not the pharmacist who’s rushing through 20 prescriptions an hour. We’re left to Google symptoms at 2 a.m., terrified, and hoping we didn’t just poison ourselves with ibuprofen because it ‘seemed harmless.’
And don’t even get me started on supplements. St. John’s wort? Sounds like something a fairy would brew. But it’s not tea-it’s a biochemical grenade. And we treat it like a yoga mat. We need a cultural shift. Not just better guidelines-better literacy. We need to stop seeing meds as ‘just pills’ and start seeing them as living, breathing, dangerous collaborators in our biology. We’re not patients. We’re ecosystems. And ecosystems don’t survive on blind trust. They survive on awareness.
Metformin and kidney disease is a big one. I’ve seen patients on it for years with eGFR of 45 and no one ever adjusted the dose. Just kept prescribing. Pharmacist flagged it three times. Doctor ignored. Until one guy ended up in ICU with lactic acidosis. Don’t assume labs are being checked. Ask. Always ask.
From a clinical pharmacology standpoint, the pharmacokinetic and pharmacodynamic interplay in polypharmacy scenarios is profoundly underappreciated in primary care. The hepatic metabolism of CYP450 substrates in the context of cirrhosis, for instance, necessitates a 30–50% dose reduction-yet adherence to such protocols remains suboptimal due to cognitive load and fragmented care coordination. Furthermore, the masking of hypoglycemic autonomic symptoms by beta-adrenergic blockade represents a high-risk phenotypic convergence between cardiovascular and endocrine pathophysiology, particularly in elderly cohorts with multimorbidity. System-level interventions, including EHR-integrated decision support with dynamic renal dosing algorithms, are urgently needed to mitigate this iatrogenic burden.
Oh my goodness. This is the most important thing I’ve read all year. I mean, I’ve had heart failure for five years, and I’ve been on ibuprofen for arthritis like it’s candy. Five years. And no one ever told me it could drown me in fluid. I thought it was just ‘a little painkiller.’ I didn’t know it was a slow-motion suicide. I feel like I’ve been walking around with a bomb in my pocket and everyone else is pretending it’s a backpack. I’m so grateful for this post. I’ve already called my doctor to switch to acetaminophen. And I’m printing out the Beers Criteria. I’m going to tape it to my fridge. This isn’t just medical advice-it’s survival.
Thank you for writing this. I am a caregiver for my mother who has diabetes, kidney disease, and depression. She takes 11 medications and three supplements. I have spent hours researching every single one. I have learned that some of the medications she was given for depression were increasing her risk of bleeding because of her history of ulcers. I showed her doctor the research. He didn’t know. He apologized. We changed the prescription. This is why we must be our own advocates. Knowledge is the only shield we have when systems fail. Please share this with everyone you know. It could save a life.
OMG I just realized my blood pressure med might be hiding my low sugar episodes 😱 I’ve been dizzy at work and thought it was stress. Turns out it’s my meds. I’m calling my doctor tomorrow. Thank you for this. I’m sharing this with my entire family. We all need to read this.
This is really well written. I’ve been on multiple meds for years and never thought about how they might affect each other. I guess I just trusted the system. I’m going to print out my list and take it to my pharmacist. Maybe they can help me sort through it. Thanks for the reminder that we need to be proactive.
As a healthcare professional in Nigeria, I can confirm that drug-disease interactions are grossly under-addressed in low-resource settings. Patients often self-medicate with antibiotics or NSAIDs because they are cheaper and accessible. Many do not have access to lab tests to monitor renal or hepatic function. The burden falls disproportionately on the elderly and those with chronic conditions. We need community-based education programs and mobile health tools that flag interactions in real time. Technology, when adapted to local contexts, can bridge the gap left by under-resourced clinics.
I used to think if a doctor prescribed it, it was safe. Then my mom had a bad reaction to a new antidepressant because she had undiagnosed liver issues. She was fine for months-then one day she couldn’t walk. Turns out the drug was building up in her system. We didn’t know. No one told us. Now I check every single thing before I take it-even OTC stuff. I’m not scared of meds-I’m just careful. And I think that’s the new normal.
Why do people not know this?! It’s not rocket science. If you have kidney problems, don’t take metformin. If you have asthma, don’t take beta-blockers. If you’re on blood thinners, don’t take ibuprofen. It’s in the damn pamphlet! People are too lazy to read. Or they trust their doctor too much. Stop being passive. Your life is not a game of Russian roulette.
This is the kind of post that should be mandatory reading in every high school health class. We teach kids how to use condoms and avoid vaping, but we don’t teach them how their bodies work with medicine. We’re raising a generation that thinks ‘natural’ means safe and ‘prescribed’ means harmless. We need to change that. Knowledge isn’t power-it’s protection. And we’re all owed that.
Let me tell you something-my uncle took lisinopril for hypertension and had a stroke because his kidneys were already failing. The doctor didn’t check his creatinine. The pharmacist didn’t say anything. He was 72. He didn’t even know he had kidney disease. Now he’s paralyzed. I’ve been asking every doctor I meet: ‘What’s the one drug that could kill me because of my other conditions?’ I ask it like a mantra. Because if you don’t ask, no one will tell you.
my grandma takes 8 pills a day. she thinks if it’s in a white capsule, it’s fine. i sat her down last week and made her read this. she cried. then she made me write down all her meds on a sticky note. now she carries it in her purse. small step. huge win.
There’s a quiet tragedy in modern medicine-we treat diseases like isolated islands, but the human body is an archipelago. One drug doesn’t just act on one system; it ripples across the entire network. We’ve built a system that rewards specialization, not integration. And so the gaps widen. The patient becomes a collection of specialists, each focused on their own piece, none seeing the whole. We need more generalists. More pharmacists in the room. More time. More listening. Because healing isn’t about fixing parts-it’s about honoring the whole.
I used to think I was just ‘getting older’ when I felt dizzy after taking my pills. Turns out my blood pressure med was making my blood sugar crash without warning. I had no idea. I thought it was just fatigue. I almost passed out at the grocery store. Now I check my glucose before I take anything. I carry glucose tabs in my purse. I’m not scared anymore-I’m prepared. And I’m telling everyone I know. This isn’t just medical info-it’s life info.