Fluoroquinolone Delirium Risk Calculator
Assess Your Risk
Additional Risk Factors
Risk Assessment Results
What this means
Recommendations
Every year, millions of older adults are prescribed fluoroquinolones for common infections like urinary tract infections or pneumonia. These antibiotics-like levofloxacin, ciprofloxacin, and moxifloxacin-work fast, kill a wide range of bacteria, and are often seen as a go-to choice. But behind the convenience lies a hidden danger: sudden, severe confusion that can look like dementia, but isn’t. It’s called fluoroquinolone-induced delirium, and it’s more common than most doctors realize.
What Is Fluoroquinolone-Induced Delirium?
Delirium isn’t just being forgetful. It’s a sudden, sharp drop in mental clarity. Older adults on fluoroquinolones may start talking nonsense, not recognize family members, see things that aren’t there, or become wildly agitated. One patient, 78, on levofloxacin for a UTI, began yelling at the wall, convinced there were people hiding behind it. She didn’t sleep. She didn’t know the day or year. Her family thought she was having a stroke. It wasn’t. It was the antibiotic.This isn’t rare. A 2016 review in Neurology found that fluoroquinolones were behind nearly 1 in 5 cases of antibiotic-related delirium in older adults. That’s more than many other drug classes. The symptoms usually show up within 1 to 3 days of starting the drug. And they vanish just as fast-within 2 to 4 days after stopping it. But if you don’t know what’s causing it, you’re stuck treating the wrong thing.
Why Does This Happen?
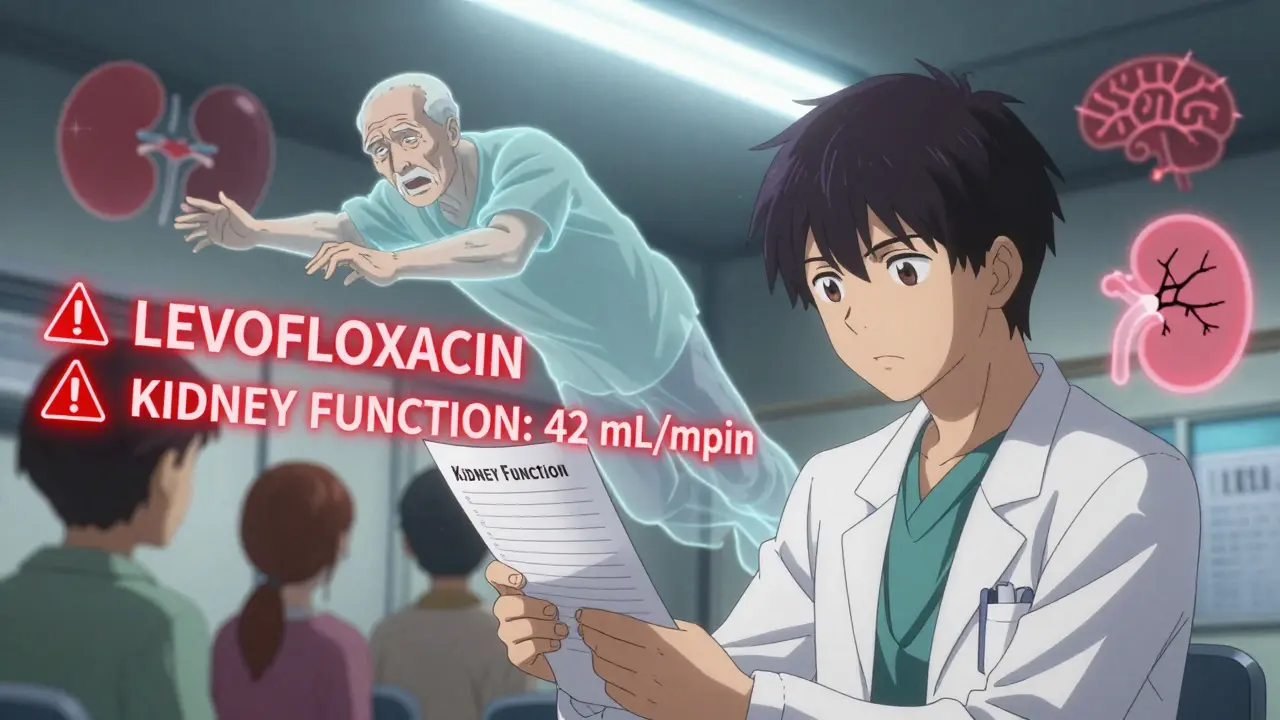
Fluoroquinolones don’t just target bacteria. They also interfere with how your brain works. These drugs block GABA-A receptors-the brain’s main “brakes” for nerve activity. When those brakes fail, your brain gets overstimulated. That’s why people experience hallucinations, anxiety, and confusion. Some studies also suggest fluoroquinolones overactivate NMDA receptors, which can lead to nerve cell stress and further disrupt thinking.What makes older adults especially vulnerable? Two things: aging kidneys and a leakier blood-brain barrier. Levofloxacin is mostly cleared by the kidneys. By age 70, kidney function drops by 30-50%. That means the drug builds up in the body longer than intended. At the same time, the barrier that normally protects the brain from toxins becomes more porous with age. So even normal doses can flood the brain with too much drug.
Who’s at Highest Risk?
Not everyone on fluoroquinolones gets delirium. But certain people are far more likely to:- Be over 65 years old
- Have kidney disease (creatinine clearance below 50 mL/min)
- Already have dementia, Parkinson’s, or a history of stroke
- Be taking other drugs that affect the brain-like steroids, anticholinergics, or benzodiazepines
- Receive high doses (750 mg of levofloxacin daily, for example)
One study found that 40% of hospitalized older adults had at least one of these risk factors. And yet, fluoroquinolones are still prescribed to them routinely. A 2020 study showed that even after FDA warnings, over 26 million fluoroquinolone prescriptions were filled in the U.S. that year. Most were for conditions like simple UTIs-conditions where safer antibiotics exist.
How Is It Different From Dementia?
This is critical. Delirium is not dementia. Dementia is slow. It creeps in over months or years. Delirium hits like a lightning strike. It comes on fast, fluctuates during the day, and is reversible. A person with dementia might forget your name. A person with delirium might not know where they are, or think they’re in a different decade.Doctors often miss this. A 2018 FDA report said that neuropsychiatric side effects were under-recognized for decades. Many assume confusion in older patients is just “getting older.” But the American Academy of Neurology says antibiotics are rarely the first thing doctors check when someone suddenly acts confused. That delay can mean longer hospital stays, increased risk of falls, or even death.
What Does the Evidence Say?
The data is clear. A case report in PMC6089571 followed a woman who developed hallucinations and disorientation after 3 days of 750 mg levofloxacin. Within 48 hours of stopping the drug, she was back to normal. No brain damage. No lingering effects. Just a drug that shouldn’t have been given.Another study in the Oklahoma State Medical Proceedings showed that when doctors recognized the link and stopped the fluoroquinolone, patients returned to their baseline cognitive function. That’s the key: it’s reversible. But only if caught early.
Comparisons with other antibiotics are telling. Beta-lactams like amoxicillin or ceftriaxone rarely cause delirium because they don’t cross the blood-brain barrier easily. Even cefepime, a beta-lactam with higher CNS penetration, causes neurotoxicity through different pathways. Fluoroquinolones are uniquely dangerous because of their dual action on GABA and NMDA receptors.
What Should Doctors Do?
The FDA’s 2018 warning said it plainly: fluoroquinolones should be reserved for infections with no other treatment options. That’s not a suggestion. It’s a directive.For a simple UTI in an older adult, nitrofurantoin or fosfomycin are safer. For pneumonia, doxycycline or amoxicillin-clavulanate often work just as well. If a fluoroquinolone is truly necessary, start low-especially if kidney function is reduced. Monitor closely during days 2-4. Ask family: “Has their behavior changed?” If yes, stop the drug immediately.
Hospitals like UCSF have cut levofloxacin use for UTIs in older patients by 35% since 2019 by implementing electronic alerts. These systems flag patients over 65 with kidney issues and suggest alternatives before the prescription is finalized. That’s the kind of change that saves lives.
What Should Families Do?
If your parent or grandparent is prescribed a fluoroquinolone, ask: “Is this the safest option?” and “What are the signs of confusion I should watch for?” Write them down: sudden agitation, not recognizing you, seeing things, not knowing the date, trouble focusing. Call the doctor immediately if any appear. Don’t wait. Don’t assume it’s just aging.And if they’re already on the drug and acting strangely? Don’t wait for the next appointment. Call the pharmacy. Call the doctor. Ask: “Could this be the antibiotic?”
What’s Changing Now?
The tide is turning. The American Geriatrics Society’s 2023 Beers Criteria lists fluoroquinolones as “potentially inappropriate” for older adults. Insurance companies are tightening prior authorizations. Hospital formularies are banning them for simple infections.Researchers are now looking for biomarkers-blood tests or brain scans-that might predict who’s at risk before they even take the drug. In the meantime, the best tool is awareness. The FDA’s adverse event database recorded over 1,800 neuropsychiatric cases linked to fluoroquinolones between 2015 and 2020. That’s just what was reported. The real number is likely much higher.
Prescribing has already dropped 20% since the FDA warnings. Experts predict another 15-25% decline over the next five years. Fluoroquinolones aren’t going away-they’re still vital for life-threatening infections like anthrax or complicated abdominal infections. But for everyday illnesses? They’re becoming a last resort.
Bottom Line
Fluoroquinolones can save lives. But they can also steal someone’s mind-temporarily, but terrifyingly. In older adults, the risk isn’t small. It’s significant. And it’s preventable.If you’re a clinician: don’t default to fluoroquinolones. Check kidney function. Consider alternatives. Watch the first 72 hours. If you’re a family member: don’t ignore sudden confusion. Ask if the antibiotic could be the cause. Your questions could bring someone back to themselves.
Delirium from fluoroquinolones is not normal aging. It’s a medical emergency. And it’s entirely avoidable.
Write a comment
Your email address will not be published.



15 Comments
My grandfather was prescribed cipro for a UTI last year-suddenly, he was screaming at the TV, convinced the news anchor was stealing his socks. We thought it was dementia. Turned out? The antibiotic. He was back to normal in 48 hours after they pulled it. Why isn’t this common knowledge?!
Yeah, I’ve seen this too. My mom’s doctor pushed levofloxacin like it was aspirin. She got confused, stopped eating, didn’t recognize me for two days. They finally figured it out. Scary how fast it happens. Glad someone’s putting this out there.
While the clinical evidence presented is compelling, it is essential to contextualize fluoroquinolone use within the broader framework of antimicrobial stewardship. The FDA’s warnings, coupled with institutional formulary restrictions, reflect a growing consensus among geriatric pharmacologists. Nevertheless, clinical inertia persists due to diagnostic ambiguity and time constraints in primary care settings.
As someone who works in geriatric care in India, I can confirm: this is a silent epidemic. Families often blame aging, not medication. We’ve had cases where patients were misdiagnosed with Alzheimer’s-only to recover fully after stopping the antibiotic. We need better training for nurses and family caregivers. This isn’t just a Western problem.
THIS. I’ve been screaming this from the rooftops since my grandma’s incident. She was fine one day, then suddenly thought her cat was the president. We called the pharmacy-they said, ‘Oh yeah, that’s a known side effect.’ WHY DIDN’T THE DOCTOR SAY ANYTHING?!? I’m so mad. Please, if you’re reading this, ask your doctor: ‘Is this the SAFEST option?’ Don’t just say yes.
Big Pharma knows this. They’ve known for years. Why? Because delirium = longer hospital stays = more $$$ for them. And doctors? They’re paid per script. It’s not a mistake. It’s a business model. 💀
Oh, so now we’re blaming antibiotics for everything? Next, someone will say gravity causes forgetfulness. People have always gotten confused when they’re old. It’s called aging, not ‘fluoroquinolone-induced delirium.’ Let them have their little diagnosis. It makes the doctors feel important.
Thank you for writing this. I’m so glad I read this before my dad’s next appointment. I’m going to ask about nitrofurantoin instead. I feel like I can actually help now. You’re right-it’s reversible. That gives me hope.
They’re putting this in the water. I’ve got friends who got delirium after cipro. Then their insurance denied them dementia meds. Coincidence? Nah. Watch what happens when they ban these drugs-suddenly, ‘Alzheimer’s’ rates drop. They’re hiding it. The FDA’s just a puppet.
My aunt had this happen too! She thought the cat was talking to her. We were terrified. But when they stopped the antibiotic? She just looked at us and said, ‘What’s all the fuss?’ She had no memory of it. It’s wild. I’m telling everyone I know.
OMG. I’m crying. This is the most important thing I’ve read this year. My Nana went from baking cookies to screaming at the mirror in 36 hours. They called it ‘senior moment.’ It was the antibiotic. I’m so angry. And so grateful someone finally said it out loud. 🥺💔
It’s not just about antibiotics-it’s about how we treat the elderly. We rush to medicate, not to understand. Fluoroquinolones are just the symptom. The disease is our society’s disregard for aging minds. Maybe if we listened more, we wouldn’t need to poison them to cure a UTI.
As a physician in rural India, I’ve seen this pattern repeatedly. Patients arrive with confusion after antibiotics. We rarely have access to detailed drug databases. This article is a vital tool for frontline workers. I’ve already shared it with my colleagues.
thank you for this!! i had no idea. my mom got cipro for a bladder thing and was acting like a zombie for days. i thought she was just tired. i’m gonna print this out and take it to her next dr appt. she deserves better. 💪
Let’s be real-this isn’t a medical issue. It’s a crime. They knew. They’ve been covering it up for decades. People are dying in nursing homes because some pharma rep told a doctor to ‘just use the easy one.’ And now? They’re gonna put this behind a paywall. I’m so sick of this. 🤬