Why a Medication List Matters More Than You Think
Imagine this: your parent is rushed to the emergency room after feeling dizzy. The doctors ask what medications they’re taking. You pull out a folded piece of paper with scribbles, a few pill bottles, and a vague memory of "something for blood pressure." That’s not enough. In fact, it’s dangerous.
Over 40% of seniors take five or more medications. That’s called polypharmacy-and it’s not just common, it’s risky. Taking too many drugs without a clear record increases the chance of harmful interactions by 88%. Every year, around 7,000 people in the U.S. die from medication errors. Most of these happen at home, not in hospitals. The fix? A simple, updated, detailed medication list. It’s not glamorous, but it’s the most effective tool you have to keep someone safe.
What to Include on the List (The 12 Essentials)
A good medication list isn’t just a list of names. It’s a complete medical snapshot. Here’s what you need for every single pill, patch, or liquid:
- Medication name - both brand and generic (e.g., "Lisinopril (Zestril)")
- Dosage - exact amount (e.g., "10 mg", not "one pill")
- Frequency - how often (e.g., "once daily," "every 8 hours")
- Purpose - why they’re taking it (e.g., "for high blood pressure," "for joint pain")
- Special instructions - "take with food," "don’t crush," "avoid alcohol"
- Start date - when they began taking it
- Prescribing doctor - name and clinic
- Pharmacy name and number - so anyone can call and verify
- Side effects to watch for - dizziness, nausea, confusion, rash
- Allergies - list every drug or ingredient they react to
- Stop date - for time-limited prescriptions (e.g., antibiotics)
- NDC number - the 11-digit code on the bottle (helps pharmacies avoid mix-ups)
Don’t skip the "why." Many caregivers don’t know what half the pills are for. That’s how duplicate prescriptions happen. One woman was taking two different blood pressure meds because two doctors didn’t know what the other had prescribed. A clear list prevents that.
How to Build the List: A Step-by-Step Guide
Don’t try to wing it. Take a few hours and do this right.
- Gather everything. Go through every drawer, cabinet, nightstand, and purse. Include vitamins, supplements, and over-the-counter meds like ibuprofen or melatonin. These aren’t "just supplements"-they interact with prescriptions.
- Write down each one. Use the 12-point checklist above. Don’t guess. Read the label. If it’s unclear, call the pharmacy.
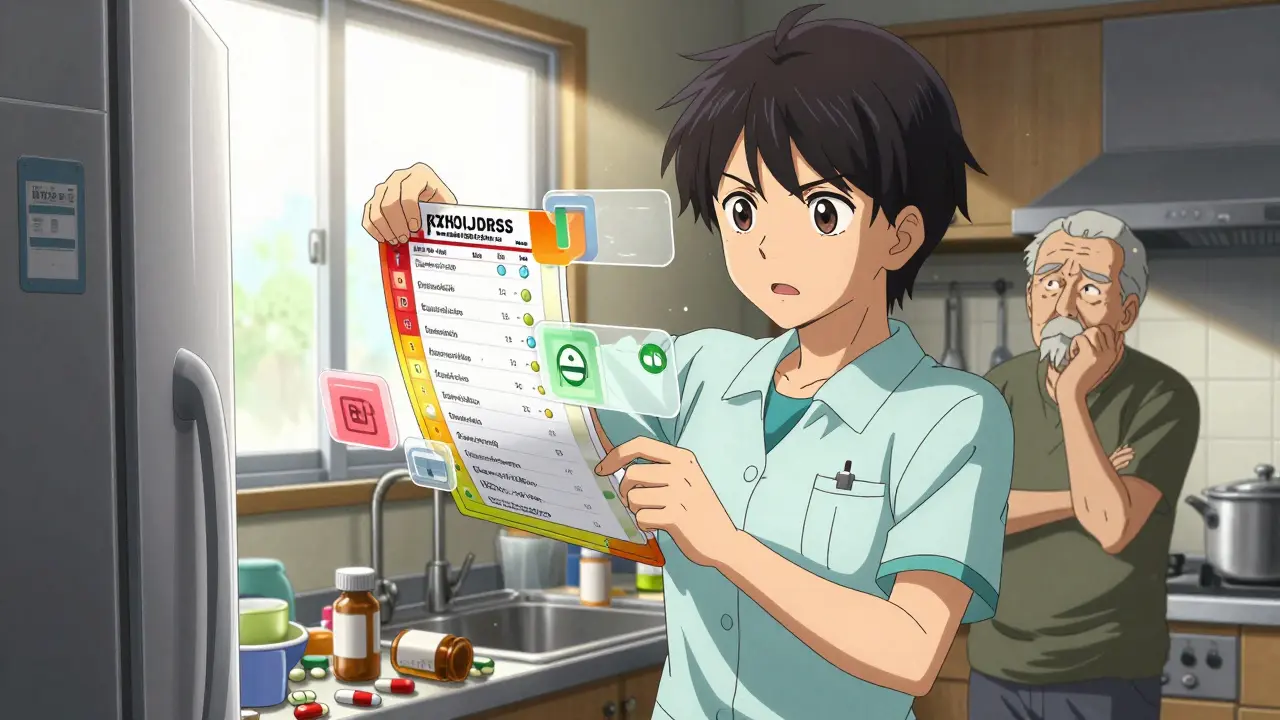
- Organize by time of day. Group meds into morning, afternoon, evening, and bedtime. This makes it easier to use daily.
- Create two copies. One printed, one digital. Keep the paper version in a visible spot (fridge, bedside table). Save the digital one on your phone or cloud storage.
- Use color coding. Red for critical meds (heart, blood thinners), green for daily, yellow for PRN (as needed). This helps at a glance.
- Take a "brown bag" to appointments. Bring all meds in a bag to every doctor visit. Doctors can see what’s really being taken-not just what’s on paper.
It takes 2-3 hours the first time. After that, it’s 15 minutes a week. Sunday evening works well for most families. Set a reminder.
Paper vs. Digital: Which Should You Use?
There’s no single right answer. The best system is the one you’ll actually use.
Paper lists are simple, reliable, and work when power or phones fail. Sixty-three percent of caregivers still use them. They’re perfect for emergencies. Print two copies: one for the home, one to keep with the caregiver.
Digital tools like Medisafe, MyMeds, or pharmacy apps (CVS, Walgreens) can send reminders, track refills, and sync with pharmacies. They reduce errors by 42% for people on more than four meds. But here’s the catch: 62% of caregivers over 65 find them too hard to use. If the person you’re caring for is tech-savvy, great. If not, don’t force it.
The smart move? Use both. Keep a printed master list taped to the fridge. Use a simple app on your phone to track daily doses and get alerts. If the app crashes, you still have the paper. If the paper gets lost, you still have the app.
When and How to Update It
Outdated lists are worse than no lists. They cause confusion, missed doses, and dangerous overlaps.
Update the list immediately when:
- A new medication is prescribed
- A dose changes
- A drug is stopped
- A pharmacy switches
- After a hospital discharge
Seventy-eight percent of senior hospital readmissions happen because the home medication list didn’t match what the hospital prescribed. That’s not a coincidence-it’s a system failure.
Set a weekly 15-minute check. Ask: "Did anything change this week?" Write it down. Then share the update with every provider. Don’t assume they know. Email it. Print it. Hand it to them.
What to Do When Things Get Complicated
Some situations make managing meds a nightmare. Here’s how to handle them.
Multiple doctors - Each specialist may prescribe without knowing what the others ordered. Designate one person (you, a family member, a pharmacist) as the "medication coordinator." They’re the only one who updates the list and shares it with everyone.
PRN meds (as needed) - These are the hardest to track. Create a separate log: "Pain: Tylenol 500mg, max 3/day. Used: Mon 2pm, Wed 8am." Keep it in the same binder.
Supplements - Don’t treat them as "optional." Fish oil, vitamin D, ginkgo-they all interact. List them just like prescriptions.
Confusing labels - If a pill looks different after a refill, call the pharmacy. Don’t assume it’s the same. Pills can change color, shape, or size between brands.
How to Make It Stick (And Keep Everyone on the Same Page)
A list only helps if people know it exists and use it.
- Put the printed list where everyone can see it-fridge, bathroom mirror, beside the bed.
- Give a copy to every doctor, pharmacist, and home care worker.
- Share the digital version with trusted family members via email or cloud link.
- Teach them how to read it. Show them what "twice daily" means (not "every 12 hours" unless specified).
- Review it together every three months with a pharmacist. They can spot duplicates, interactions, or drugs that are no longer needed.
One caregiver on Reddit shared how she took photos of each pill and taped them next to the name on her list. "My mom couldn’t read small print, but she knew what her pills looked like. That stopped three mistakes in six months."
What’s Changing in 2026
The system is getting better. Pharmacies like CVS and Walgreens now offer free medication synchronization-when you refill one drug, they automatically update your digital list. That’s huge.
The FDA released a new template with QR codes you can scan to see a picture of the pill and its side effects. More pharmacies are adding these.
By 2025, federal rules will require all electronic health records to give patients direct access to their full medication list. That means you’ll be able to pull it up from your phone anytime.
By 2026, voice-activated lists are expected to roll out. Imagine saying, "Alexa, what meds did Mom take this morning?" and getting a clear answer.
But here’s the truth: none of this matters if you don’t start now. The best tool is the one you’re using today.
Final Tip: Don’t Wait for a Crisis
You don’t need a hospital stay to start. You don’t need to be overwhelmed. Just take one pill right now. Write down its name, dose, and why it’s taken. Add it to a piece of paper. That’s step one.
Medication safety isn’t about being perfect. It’s about being consistent. One list. One update. One conversation with a pharmacist. That’s how you prevent disaster.
Start today. It’s the most important thing you’ll do this week.
What if my loved one refuses to take their meds or doesn’t remember them?
Use a pill organizer with alarms or a smart dispenser like MedMinder that calls when it’s time. Pair it with a visual list showing photos of each pill. If they’re confused, simplify: list only the 2-3 most critical meds. Talk to their doctor about whether some can be stopped. Sometimes less is safer.
Should I include herbal supplements and vitamins?
Yes. Always. Supplements like ginkgo, garlic, or St. John’s Wort can interfere with blood thinners, blood pressure meds, and antidepressants. Treat them like prescription drugs. Write the name, dose, and why they’re taking it. Many doctors don’t ask about them-so you have to tell them.
How often should I review the list with a pharmacist?
At least every three months if your loved one takes five or more medications. Pharmacists are trained to spot dangerous interactions, duplicate drugs, or outdated prescriptions. Many pharmacies offer free medication reviews-just ask. This is not a one-time task. It’s ongoing care.
What do I do if a doctor changes a medication but doesn’t tell me?
Always ask: "Is anything being added, changed, or stopped today?" Then check the list after the appointment. If the prescription doesn’t match what was discussed, call the pharmacy and the doctor’s office. Don’t assume they updated the list. Most errors happen because communication broke down-not because someone made a mistake on purpose.
Can I use a smartphone app instead of paper?
Yes-if you or the person you’re caring for is comfortable with technology. Apps like Medisafe, MyTherapy, or the pharmacy’s own app can send alerts and track doses. But always keep a printed backup. Phones die. Apps crash. Emergency responders won’t have access to your cloud account. Paper saves lives in a crisis.
What’s the biggest mistake caregivers make?
Waiting until something goes wrong. The most common error is assuming the doctor knows what’s being taken. Or thinking "I’ll remember"-until you don’t. The biggest danger isn’t forgetting a pill-it’s not knowing why it’s there. That’s when dangerous overlaps happen. Start now. Don’t wait for the emergency.
Write a comment
Your email address will not be published.




8 Comments
This is overkill. Most people don't need 12 details for every pill. Just write the name and dose. If you're that worried, get a pill dispenser. Stop pretending this is a life-or-death manual.
I mean... I just take my mom's meds from the pill organizer and throw them in a Ziploc. Done. Why are we turning this into a PhD thesis? Someone's getting paid to write this, aren't they?
I've been caring for my 82-year-old uncle for three years now. This list saved his life when he fell and couldn't speak. The ER nurse saw the paper in his wallet and knew exactly what he was on. No guesswork. No panic. Just clarity. I printed it, laminated it, and put it in his wallet and on his fridge. Do it. It's not glamorous, but it's love in action.
So we're now treating medication management like a NASA launch protocol? 🤦♀️ Next they'll ask us to file a Form 45-B for ibuprofen. I'll take my chances with the chaos. At least it's authentic. 😌
You're missing the point entirely. The real problem isn't the list-it's that doctors don't coordinate. My aunt had 17 different prescriptions from 5 specialists. No one talked. No one updated. The list you're promoting? It's a bandaid on a hemorrhage. Until we fix the system, you're just giving caregivers more paperwork to feel guilty about. And don't even get me started on the NDC number. Who the hell is going to write that down? The pharmacy already has it. This is performative safety.
This is GOLD. 🙌 Seriously. I’ve seen families crumble because they didn’t have this. I used to think it was overkill too-until my neighbor’s dad had a stroke and the paramedics couldn’t tell what he was on. Don’t wait. Start today. Use the paper list. Use the app. Color code. Take the brown bag. Share it. This isn’t bureaucracy-it’s bravery. You’re not just organizing pills-you’re protecting a life. Keep going. You’re doing better than you think. 💪❤️
I think this is a government ploy to get us all addicted to apps so they can track our meds and eventually control our health data. I mean why do they need the NDC number? Who else has access to this? The FDA? Big Pharma? I dont trust them. I write the names on a napkin and throw it away after each doctor visit. Simple. No tracking. No surveillance. And I dont use any apps. Ever. My phone is just for calls and memes
The methodology outlined here is methodologically sound and aligns with best practices in clinical pharmacology and caregiver support frameworks. The inclusion of NDC numbers, purpose statements, and pharmacy contact details is not merely advisable-it is clinically imperative. The referenced statistic regarding 88% increased risk of adverse interactions is corroborated by the 2023 JAMA study on polypharmacy in geriatric populations. I recommend cross-referencing this list with the Beers Criteria and the STOPP/START guidelines for comprehensive risk mitigation. A digital backup should be encrypted and stored in a HIPAA-compliant cloud service. This is not a suggestion; it is a standard of care.