
Medication Rash Risk Assessment
What do your symptoms look like?
This assessment helps determine if your rash requires urgent medical attention. Based on information from the article.
More than one in five people taking prescription drugs will develop a skin rash at some point. Most of these are harmless and go away on their own. But some can turn deadly in days. If you’ve noticed red bumps, itchy patches, or blisters after starting a new medication, you’re not alone. And you need to know what to do next.
Not All Rashes Are the Same
Drug rashes aren’t one thing. They come in many forms, and each tells a different story. The most common is the morbilliform rash - small, red, flat spots that look like measles. It usually shows up 1 to 2 weeks after starting a new drug, often on the chest, back, or arms. This type accounts for 90% of all medication-related rashes and almost never turns dangerous. It just means your body reacted to something, and stopping the medicine usually makes it vanish in 1 to 2 weeks.
Then there’s urticaria - hives. These are raised, itchy welts that can pop up anywhere, even within an hour of taking a pill. They come and go fast. If they disappear in 24 to 48 hours after stopping the drug, it’s likely a mild reaction. But if they keep coming back, or if your lips or tongue swell, that’s a red flag.
Some rashes look like coins - round, red, scaly patches called nummular dermatitis. Doctors often mistake these for eczema. But if they appeared after you started a new antibiotic or blood pressure pill, and they clear up quickly after stopping it, you’re likely dealing with a drug-induced version. Unlike regular eczema, which can last for years, drug-triggered nummular dermatitis usually fades in 4 to 8 weeks.
The Dangerous Ones You Can’t Ignore
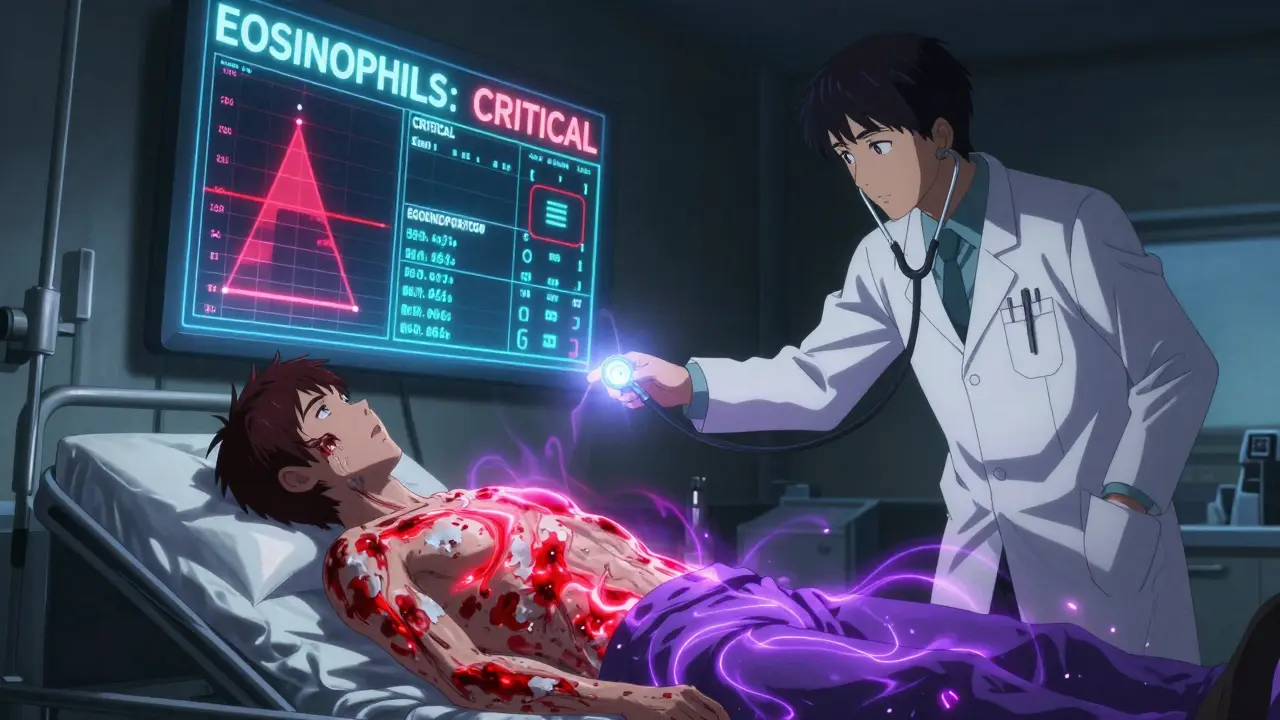
While most rashes are mild, a few are medical emergencies. Three stand out: Stevens-Johnson Syndrome (SJS), Toxic Epidermal Necrolysis (TEN), and DRESS syndrome.
SJS and TEN are on the same spectrum - they start with flu-like symptoms, then the skin begins to blister and peel, like a bad burn. SJS affects less than 10% of the body. TEN affects more than 30%. Both require hospitalization. About 1 in 10 people with SJS don’t survive. For TEN, that number jumps to 1 in 3.
DRESS - Drug Reaction with Eosinophilia and Systemic Symptoms - is sneakier. It doesn’t just hit the skin. It can wreck your liver, kidneys, or lungs. It usually shows up 2 to 6 weeks after starting a drug. You might feel tired, have a fever, swollen glands, or swollen face. Blood tests will show high eosinophils - a type of white blood cell that spikes when your body is overreacting. The worst part? You might not realize the drug is the cause. It could be something you’ve taken for months.
Common triggers for DRESS include:
- Carbamazepine (for seizures)
- Phenytoin (another seizure drug)
- Lamotrigine (used for epilepsy and bipolar disorder)
- Allopurinol (for gout)
- Sulfonamide antibiotics (like Bactrim)
- Minocycline (an acne antibiotic)
If you’re on any of these and develop a rash, don’t wait. Call your doctor today.
Who’s at Highest Risk?
It’s not random who gets a bad reaction. Certain people are far more likely to have serious skin reactions.
If you’re taking five or more medications, your risk of a drug rash jumps to 35%. That’s seven times higher than someone on just one or two pills. This is why older adults - who often take multiple prescriptions - are the most common group affected.
People with certain genetic markers are at extreme risk. In Southeast Asia, carrying the HLA-B*1502 gene makes you 1,000 times more likely to develop SJS from carbamazepine. In Han Chinese populations, HLA-B*5801 increases allopurinol-related SCAR risk by 580 times. Some doctors now test for these genes before prescribing - especially in high-risk groups.
Having a viral infection like Epstein-Barr (mononucleosis) or HIV while taking antibiotics? Your risk of a bad rash goes up 5 to 10 times. Cancer patients on chemotherapy also have 3 to 5 times higher risk. And if you’ve had a drug rash before, you’re far more likely to get another - even from a different medicine.
What Medications Cause the Most Rashes?
Some drugs are far more likely to cause skin reactions than others. Here’s who’s on the top list:
- Penicillin antibiotics - Cause 10% of all drug rashes. They’re also responsible for 80% of severe allergic reactions.
- NSAIDs (ibuprofen, naproxen) - Cause 25% of non-allergic drug reactions. These aren’t always immune-related - they can irritate the skin directly.
- Anticonvulsants (carbamazepine, phenytoin, lamotrigine) - Linked to DRESS and SJS/TEN. Lamotrigine alone causes rashes in up to 10% of users.
- Allopurinol - The #1 drug linked to DRESS and SJS in older adults, especially those with kidney problems.
- Sulfonamides (Bactrim, Septra) - Cause 8% of all drug rashes. High risk if you have HIV.
- Chemotherapy drugs - Nearly every one can cause some form of rash. Some are predictable; others are random.
Also watch out for photosensitivity. Some drugs make your skin burn in sunlight. Doxycycline, ciprofloxacin, and hydrochlorothiazide are common culprits. If you get a bad sunburn after taking one of these - even with sunscreen - it might not be sunburn at all.
What Should You Do If You Get a Rash?
Don’t panic. But don’t ignore it either.
If it’s mild: Small red spots, mild itching, no fever, no blisters. Stop the new medication only if your doctor says to. Many rashes clear up on their own. In the meantime, use lukewarm water for showers, avoid soap, and apply a 1% hydrocortisone cream twice a day. Moisturize within 3 minutes of bathing. Keep the skin cool and dry.
If it’s serious: Blisters, peeling skin, fever over 38°C, swelling of the face or throat, trouble breathing, or sores in your mouth or eyes? Go to the emergency room now. Don’t call your doctor. Don’t wait. This isn’t a next-day appointment. This is a life-or-death situation.
Never stop critical meds on your own. If you’re on a seizure drug like carbamazepine, stopping suddenly can cause a seizure. If you’re on blood pressure or heart meds, stopping could trigger a stroke or heart attack. Always talk to your doctor first. They might switch you to a safer alternative.

How Doctors Figure Out What’s Causing It
Pinpointing the exact drug is harder than you think. Most people take multiple medications. Your doctor might have to stop them one by one - a process that can take weeks. That’s why they often rely on timing. Did the rash appear 10 days after starting a new drug? That’s a clue. Did it show up 3 weeks later? That points to DRESS. Did it appear within an hour? That’s likely an IgE-mediated allergy.
Testing has improved. Skin tests for penicillin allergy are now 95% accurate. Blood tests can check for eosinophils and liver enzymes. Genetic testing is becoming more common for high-risk drugs. But there’s still no perfect test for most drug rashes. It’s often detective work.
One big myth: if you had a rash from penicillin as a kid, you’re probably not allergic anymore. Studies show 15% of people who think they’re allergic to penicillin can actually take it safely. A simple skin test can clear this up.
How to Prevent Future Rashes
Keep a list of every drug you’ve ever had a reaction to - even if it was years ago. Include the name, what the rash looked like, and when it happened. Share this with every new doctor.
If you’ve had one drug rash, assume you’re at higher risk for others. Avoid drugs in the same class. For example, if you reacted to one sulfa drug, avoid all sulfa antibiotics.
Ask your pharmacist: “Is this new medicine known to cause skin reactions?” They’re trained to spot these risks.
If you’re on multiple drugs, ask your doctor if any can be reduced or replaced. Fewer pills = lower risk.
And if you’re over 65? Be extra cautious. Your body processes drugs slower. Your skin is thinner. Your immune system is less predictable.
Bottom Line
Most drug rashes are annoying, not dangerous. But you can’t afford to guess. If you notice something new on your skin after starting a medicine - especially if it’s spreading, blistering, or accompanied by fever - act fast. Talk to your doctor. Don’t wait. Don’t assume it’s just a rash. It could be the early sign of something life-threatening. And if you’ve had one before? You’re not just unlucky. You’re at risk. Stay informed. Stay alert. Your skin is your body’s warning system. Listen to it.
Write a comment
Your email address will not be published.




1 Comments
Drug-induced skin reactions are a classic example of idiosyncratic adverse drug reactions (ADRs), which are non-dose-dependent and often mediated by immune mechanisms. The morbilliform eruption, which accounts for ~90% of cases, is typically T-cell mediated with delayed hypersensitivity (Type IV), whereas urticaria and anaphylactoid reactions involve IgE (Type I). The real clinical challenge lies in distinguishing between benign reactions and severe cutaneous adverse reactions (SCARs) like SJS/TEN and DRESS, which carry mortality rates of 5–30% and 5–10% respectively. Key diagnostic clues include the latency period-DRESS typically manifests 2–6 weeks post-exposure-and the presence of systemic involvement: fever, lymphadenopathy, eosinophilia, and hepatic transaminitis. Genetic screening for HLA-B*1502 (carbamazepine) and HLA-B*5801 (allopurinol) is now standard of care in high-risk populations, per CPIC guidelines. Early withdrawal of the offending agent is critical, but in DRESS, corticosteroids are often required due to prolonged inflammation.