
Autoimmune thyroid eye disease, also known as thyroid eye disease (TED) or Graves’ orbitopathy, isn’t just about dry eyes or puffiness. It’s a serious condition where your immune system attacks the tissues around your eyes-muscles, fat, and connective tissue-causing swelling, pain, and sometimes permanent vision damage. If you’ve been told you have ‘allergies’ or ‘sinus issues’ but your eyes keep bulging, hurting, or double-vision won’t go away, you might be dealing with something far more complex.
What Exactly Is Thyroid Eye Disease?
Thyroid eye disease is an autoimmune disorder closely linked to Graves’ disease, where the body produces antibodies that mistakenly target the thyroid gland. But here’s the twist: those same antibodies also bind to receptors in the eye socket, triggering inflammation. About 90% of TED cases happen in people with hyperthyroidism, though it can also show up in those with underactive thyroids-or even normal thyroid levels. The American Thyroid Association estimates that one in three people with Graves’ disease will develop eye symptoms, usually within six months of their diagnosis.
It’s not rare-it affects 90 to 300 people per 100,000. But because symptoms start slowly, many wait months before getting the right diagnosis. Primary care doctors often mistake it for allergies or sinus infections. The thyroid eye disease timeline is key: it has two phases. First, an active inflammatory phase that lasts one to three years, where swelling and redness flare up. Then, an inactive phase where the inflammation settles, but the damage-like bulging eyes or double vision-stays.
Common Symptoms You Can’t Ignore
The symptoms of TED don’t always start with obvious bulging. Many people first notice grittiness, like sand in their eyes, or excessive tearing. Light sensitivity, redness, and pain behind the eyes-especially when looking up or down-are early red flags. About 78% of patients report that gritty feeling, and 65% deal with dry or watery eyes. Around half of those with moderate to severe cases develop double vision because the eye muscles swell and stick, making it hard for the eyes to move together.
One of the most recognizable signs is eyelid retraction. Your eyelids pull back, giving you a wide-eyed, startled look-even when you’re not paying attention. About 45% of patients can’t fully close their eyes at night, which leads to corneal exposure. In 15-20% of severe cases, that exposure turns into painful ulcers or infections. And in the worst cases, the swollen muscles press on the optic nerve, leading to vision loss. Color vision changes are often the first warning sign of nerve compression.
It’s usually worse in one eye than the other. In 70% of cases, one eye is 30-40% more affected. That asymmetry makes it easy to dismiss as something minor-until it isn’t.
How Is It Diagnosed?
Diagnosing TED isn’t just checking your thyroid levels. It’s a full eye exam paired with thyroid testing. Doctors look for:
- Thyroid function tests (TSH, free T4, free T3)
- Anti-TSHR antibody levels-high levels match up with more severe eye disease in 75% of cases
- Visual field tests and OCT scans to check nerve health
- Orbital CT or MRI to see swollen muscles
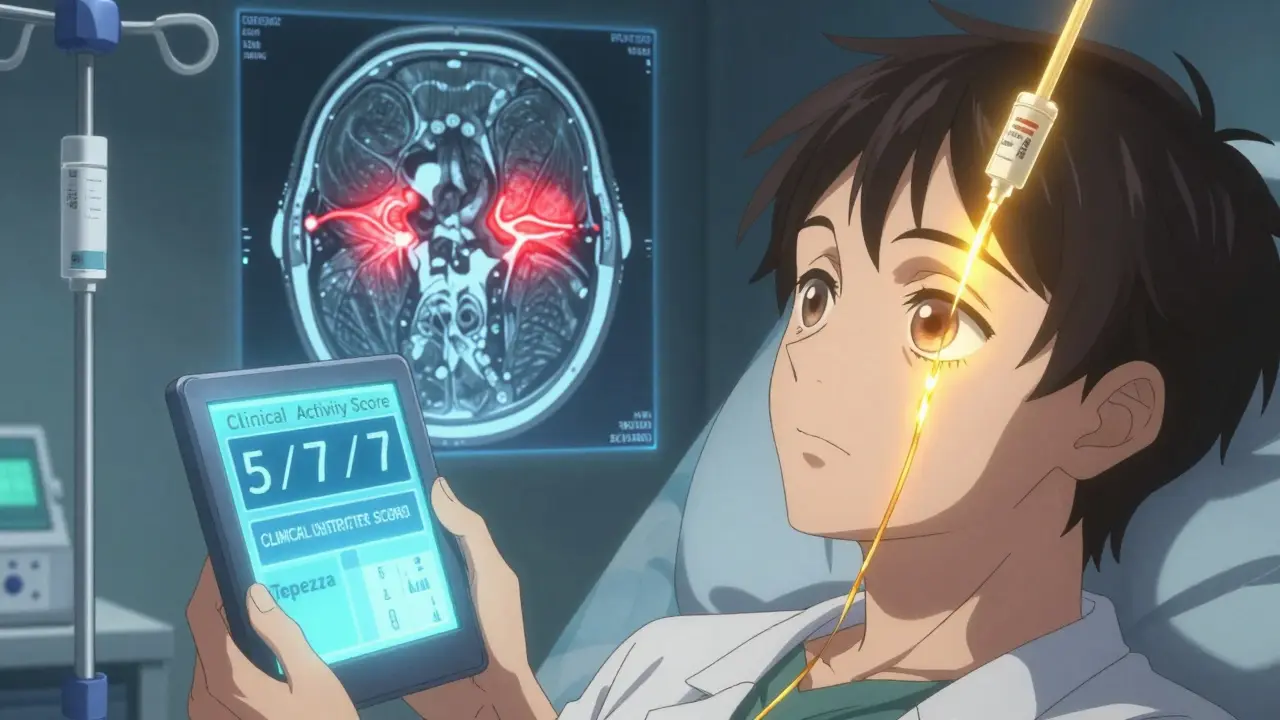
The medial rectus muscle (which moves the eye inward) is affected in 90% of cases. The inferior rectus follows at 75%. These patterns help confirm the diagnosis. A key tool is the Clinical Activity Score (CAS), which counts signs of inflammation: redness, swelling, pain with movement, and more. A score of 3 or higher means the disease is still active-and that’s when treatment needs to start.
But here’s the problem: only 45% of community ophthalmologists consistently use the CAS. At major centers, it’s 89%. That gap means many people are diagnosed too late.
Current Treatments: From Supplements to Breakthrough Drugs
Treatment depends on how active and how severe the disease is. For mild cases, selenium supplements (100 mcg twice daily) can reduce progression by 35%, according to a major European trial. It’s simple, safe, and often the first step.
For moderate to severe active TED, the old standard was high-dose IV steroids-methylprednisolone, given weekly for 12 weeks. It works for 60-70% of people, but side effects are real: liver damage in 15%, high blood sugar in 25-30%. And steroids don’t fix the bulging eyes-they just calm the inflammation.
Then came Tepezza (teprotumumab). Approved by the FDA in January 2020, it was the first drug made specifically for TED. It blocks the IGF-1 receptor, which plays a big role in the inflammation and tissue growth behind the eyes. In clinical trials, 71% of patients saw their bulging eyes reduce by at least 2 mm-compared to only 20% on placebo. Double vision improved in 68% of those treated, versus 29% on placebo.
It’s given as eight infusions, every three weeks. Each dose costs about $5,500, so the full course runs around $44,000. Insurance often denies it at first-35% of initial requests get rejected. But for many, it’s life-changing. Patients report being able to drive again, no longer needing to wear sunglasses indoors, and feeling less self-conscious.
Side effects? Muscle cramps are common (65% of users), and some report hearing loss-though that’s rare. The FDA now requires doctors to monitor hearing during treatment.
Surgery: When Medication Isn’t Enough
After the active phase ends, surgery becomes an option to fix what’s left behind. If your eyes still bulge, you might need orbital decompression surgery-removing bone from the eye socket to create more space. Endoscopic approaches now make up 65% of these procedures because they’re less invasive and have fewer complications.
If double vision won’t go away, strabismus surgery repositions the eye muscles. It helps 30-40% of patients. For eyelids that won’t close properly, eyelid retraction surgery restores a natural look-and protects the cornea. Success rates are 75-85% when done at least six months after inflammation stops.
But here’s the catch: 20% of patients need more than one surgery. The eye changes over time, and each problem needs its own fix. That’s why coordination between endocrinologists, ophthalmologists, and surgeons matters.
The Biggest Risk Factor: Smoking
No matter how advanced the treatment, smoking makes TED worse. Smokers are 7.7 times more likely to develop TED-and twice as likely to get the severe form. Quitting is the single most effective thing you can do. It doesn’t just reduce your risk-it makes treatments work better. Studies show smokers respond less to steroids and Tepezza than non-smokers.
And it’s not just about quitting for your eyes. Smoking also worsens thyroid disease overall. If you have Graves’ disease and smoke, your odds of developing TED go up dramatically. Stopping smoking is as important as any drug.

What’s Next? The Future of TED Treatment
Tepezza changed everything-but it’s not the end. The European Medicines Agency approved it for teens as young as 12 in June 2023. New drugs are in the pipeline: rituximab shows promise for patients who don’t respond to Tepezza, and a biosimilar version (teprotumumab-trbw) is expected in 2025. Researchers are also testing satralizumab, which blocks IL-6, a key inflammation signal.
Scientists are working on biomarkers to predict who will respond best. For example, if your anti-TSHR antibody level is above 15 IU/mL, you’re 80% likely to respond well to Tepezza. That could mean personalized treatment instead of trial and error.
The long-term goal? Preventing TED before it starts. Some labs are developing vaccines that target the TSHR antibodies before they attack the eyes. It’s early, but if it works, it could change Graves’ disease from a lifelong condition to something manageable before eye damage ever happens.
Life With TED: The Hidden Toll
Behind the medical facts are real lives. A 2022 survey found 74% of TED patients had anxiety or depression. Over half said they struggled to drive at night because of double vision. Sixty-three percent felt embarrassed by their appearance. Some lost jobs. Others were passed over for promotions because people assumed they were angry or unfriendly.
One woman, after 18 months of double vision, regained her ability to drive after Tepezza. Another man lost vision permanently because his optic nerve compression was missed for too long. These aren’t rare cases-they’re warnings.
The average patient waits over six months to get the right diagnosis. That delay can mean the difference between recovery and permanent damage. If you have Graves’ disease and your eyes feel off, don’t wait. See an ophthalmologist who specializes in thyroid eye disease. Many major hospitals now have dedicated TED clinics that cut diagnosis time by over a month.
When to Act
If you notice any of these signs-bulging eyes, persistent redness, pain with movement, double vision, or eyelids that won’t close-you need help now. The window for the best results is within the first 12 months of symptoms. After that, the inflammation fades, but the damage stays.
Start with your endocrinologist and ask for a referral to a thyroid eye specialist. Don’t settle for ‘it’s just allergies.’ Document your symptoms. Take photos. Track when they started and how they’ve changed. Use apps like TED Tracker to monitor your Clinical Activity Score. And if you smoke-stop today. It’s not just advice. It’s your best defense.
Thyroid eye disease is no longer a mystery. We have tools now-better drugs, smarter surgery, earlier diagnosis. But they only work if you act fast.
Can thyroid eye disease cause permanent vision loss?
Yes, in severe cases, swelling of the eye muscles can compress the optic nerve, leading to vision loss. Early signs include color vision changes and blurred vision. If left untreated, this can become permanent. That’s why prompt diagnosis and treatment during the active phase are critical.
Is Tepezza covered by insurance?
Tepezza is FDA-approved and covered by most major insurance plans, but prior authorization is often required. About 35% of initial requests are denied, usually because insurers want proof of disease severity or failed steroid treatment. Working with a specialist who documents your Clinical Activity Score and imaging results improves approval chances.
Does thyroid eye disease go away on its own?
The active inflammation phase usually lasts 1-3 years and then slows down, but the damage-like bulging eyes, eyelid retraction, or double vision-does not reverse on its own. Without treatment, these changes can become permanent. Early intervention can prevent long-term issues.
Can you get thyroid eye disease without Graves’ disease?
Yes, though it’s rare. About 10% of TED cases occur in people with normal thyroid function or hypothyroidism. The same autoimmune antibodies that target the thyroid can also attack eye tissues, even when thyroid hormone levels are balanced.
How long does Tepezza treatment take?
Tepezza is given as eight intravenous infusions, one every three weeks. The full course takes about 20-22 weeks, or roughly five months. Most patients see improvements in eye bulging and double vision within the first few infusions, with full results typically seen by the end of treatment.
Are there natural remedies for thyroid eye disease?
Selenium supplements have been proven to reduce progression in mild cases. Other supplements or home remedies have no strong evidence. Quitting smoking, using artificial tears, and sleeping with your head elevated can help manage symptoms-but they don’t treat the underlying autoimmune process. Always consult your doctor before trying anything beyond proven therapies.
Can thyroid eye disease come back after treatment?
Once the active phase ends, the disease usually doesn’t flare again. However, residual damage like eye bulging or double vision may require surgery. In rare cases, inflammation can return, especially if thyroid levels become unstable or if the patient resumes smoking. Long-term follow-up with an eye specialist is recommended.
Write a comment
Your email address will not be published.


9 Comments
my eyes have been burning for months and my doctor kept saying it was allergies... i finally saw a specialist and they were like ohhh that’s TED. i cried. it’s real. thank you for writing this.
The clinical data presented here is both comprehensive and clinically relevant. The emphasis on the Clinical Activity Score as a diagnostic tool is particularly noteworthy, given its underutilization in community settings. A standardized protocol for early referral could significantly reduce long-term morbidity.
if you’re reading this and you’ve been told it’s just dry eyes-don’t let that slide. i had double vision for 8 months before someone listened. Tepezza didn’t fix everything, but it gave me back my life. you’re not overreacting. your symptoms matter. go see a TED specialist. now.
it’s wild how something so invisible to others can change your whole world. i used to avoid mirrors. now i can drive at night again. small wins matter. keep going, everyone. you’re not alone in this.
everyone’s acting like Tepezza is magic but it’s just another expensive steroid with a fancy name. 44k? really? and you still need surgery after? this is capitalism exploiting sick people. also, smoking? duh. newsflash: everything’s worse if you smoke.
bro i got TED and i don’t even have Graves’ 😳 i was normal thyroid and then boom-bulging eyes. now i’m on Tepezza. 65% muscle cramps? yeah that’s real. also 🤕
my sister had this and no one believed her until her eye started bleeding from not being able to close it. please if you’re reading this and your eyes hurt-get checked. i wish someone told me sooner
as someone who moved from Nigeria to the US and went through this alone-i want to say: you’re not broken. you’re not dramatic. you’re fighting an invisible war. Tepezza saved my vision. Quitting smoking saved my soul. you’ve got this.
when the docs told me it was "just stress"... i nearly lost my eyesight. now i’m on Tepezza and my face looks like me again. i used to wear sunglasses indoors. now i smile in selfies. this ain’t just medicine-it’s resurrection. 🙏👁️🔥