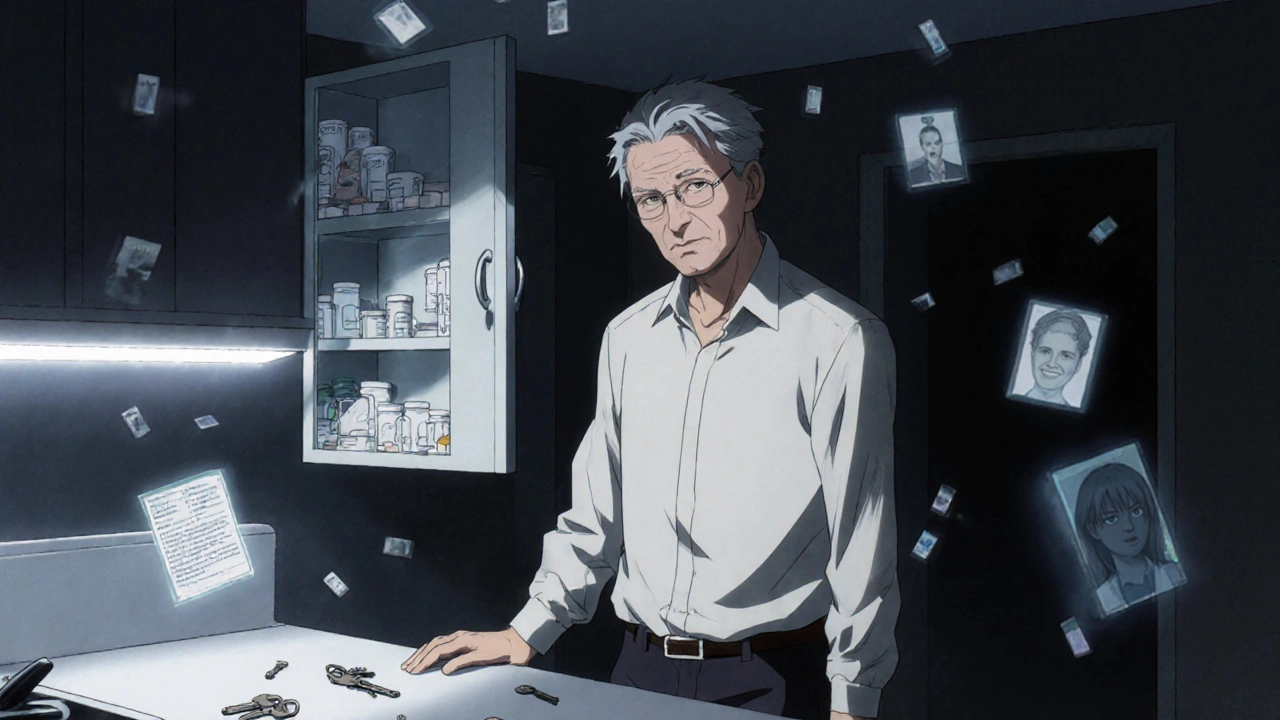
Every year, millions of people take benzodiazepines for anxiety, insomnia, or seizures. But what most don’t realize is that these drugs don’t just calm the mind-they can quietly erode memory, increase the chance of a dangerous fall, and make quitting harder than expected. If you’ve been on them for months or years, the effects may already be showing up: forgetting where you put your keys, stumbling on flat ground, or feeling mentally foggy even when you haven’t taken a pill in hours.
How Benzodiazepines Hurt Memory
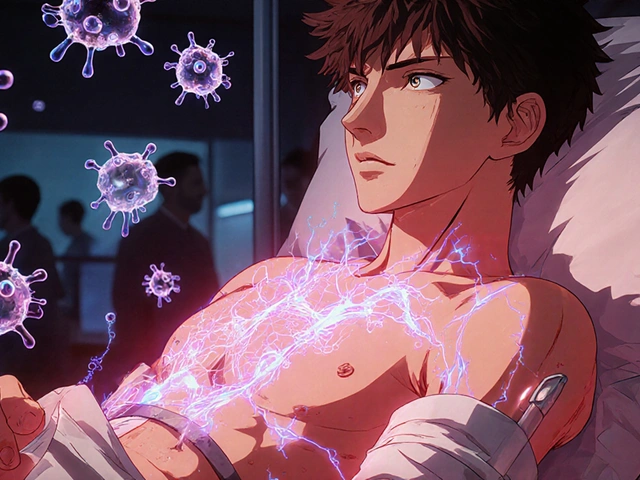
Benzodiazepines like diazepam, lorazepam, and alprazolam work by boosting GABA, a brain chemical that slows down nerve activity. That’s why they help with anxiety and sleep. But this same mechanism blocks the brain from forming new memories. This isn’t just temporary forgetfulness-it’s anterograde amnesia, meaning you can’t lay down new memories after taking the drug. Studies show this happens even at low doses, and it gets worse with higher doses or longer use. The hippocampus, the brain’s memory center, is especially sensitive. When benzodiazepines bind to receptors there, they disrupt how information moves from short-term to long-term storage. You might remember what you had for breakfast, but not what you talked about five minutes later. Complex tasks-like following a recipe, learning a new route, or remembering names-are hit hardest. Simple things, like recognizing a face, are less affected. Long-term users show measurable declines across multiple cognitive areas. A 2023 review of 19 studies found that people using benzodiazepines for over a decade had worse working memory, processing speed, attention, and visuospatial skills. On average, their IQ dropped by 10 to 15 points. Reaction times slowed by 15-25%. These aren’t small changes-they affect driving, managing medications, and even cooking safely. Worse, these problems don’t vanish when you stop. Six months after quitting, many still struggle with memory and focus. One study tracking people for 10 months found only 45% returned to normal cognitive function. The rest kept battling brain fog, trouble concentrating, and delayed thinking. Brain scans show no permanent damage, but the brain’s ability to process information efficiently hasn’t fully recovered.Why Benzodiazepines Increase Fall Risk
Falls aren’t just accidents-they’re medical emergencies, especially for older adults. Benzodiazepines make falls far more likely. A 2014 analysis of over a million people found users had a 50% higher chance of falling and a 70% higher risk of breaking a hip. These aren’t rare outcomes. In the U.S. alone, benzodiazepines contribute to about 93,000 emergency room visits for falls each year. The reasons are physical, not just mental. These drugs reduce balance control by 30-40% and slow reaction times by 25-35%. Standing up quickly, stepping over a rug, or catching yourself on a slippery floor becomes much harder. High-potency drugs like alprazolam and lorazepam are riskier than longer-acting ones like diazepam. Even people who feel fine can be at risk-many don’t realize how much their coordination has slipped. The American Geriatrics Society has listed benzodiazepines as inappropriate for older adults since 2012. Why? Because the risks outweigh the benefits. For someone over 65, the chance of a fall-related injury is higher than the chance of lasting anxiety relief. And once a fall happens, recovery is slower, complications are more common, and independence often doesn’t return.Tapering Off: The Only Safe Way Out
Stopping benzodiazepines cold turkey is dangerous. Withdrawal can trigger seizures, extreme anxiety, hallucinations, and even psychosis. That’s why tapering isn’t optional-it’s essential. But not all tapers are created equal. The gold standard is the Ashton Protocol, developed by neuropharmacologist Dr. C. Heather Ashton. It recommends reducing your dose by 5-10% every 1-2 weeks. For long-term users, even slower is better-sometimes just 2-5% per month. Switching from a short-acting drug like alprazolam to diazepam (which has a longer half-life) makes the process smoother and reduces withdrawal spikes. A 2021 trial with 312 long-term users showed that a 12- to 16-week taper using diazepam led to 68.5% successfully quitting after six months. That’s more than double the success rate of those who didn’t taper. But it’s not easy. About 22% needed to pause their taper for a few weeks because symptoms got too intense. Eight percent quit entirely because it was too hard. The good news? Cognitive improvement starts early. Within four weeks of tapering, many report clearer thinking. By eight weeks, processing speed and attention improve by 15-18%. People who stick with it often say their memory, focus, and energy return over 6-12 months. One user on a major support forum wrote: “I thought I was broken. After 10 months off, I remembered how to read a book without rereading the same paragraph five times.”
What Works in Real Life
People who succeed at tapering share a few habits:- They use diazepam as a switch. It’s easier to measure small reductions because it comes in 2mg, 5mg, and 10mg tablets.
- They track symptoms with apps like BrainBaseline or even a simple journal. Writing down daily focus, mood, and memory helps spot patterns.
- They go slow. Cutting 10% every two weeks sounds fine on paper, but many need to hold at one dose for a month or more.
- They avoid alcohol, sleep aids, and other CNS depressants. Mixing them increases sedation and fall risk.
- They get support. Online communities like the Benzodiazepine Information Coalition have over 15,000 members who share tapering tips and encouragement.
When to Consider Staying On
Not everyone needs to quit. Some people with severe epilepsy, treatment-resistant anxiety, or chronic muscle spasms benefit long-term. But even then, guidelines are clear: use the lowest effective dose. For adults under 65, that’s no more than 10 mg of diazepam daily. For those over 65, it’s 5 mg or less. Doctors should screen for cognitive decline every six months using the MoCA or MMSE. If a patient’s score drops by 2-3 points, it’s a red flag. That’s not normal aging-that’s drug effect. And while most people decline over time, some don’t. A 2023 study found about 30% of older adults on long-term benzodiazepines showed little to no cognitive decline. Researchers think genetics, lifestyle, or brain resilience may play a role. But that’s not a reason to keep taking them blindly. It’s a reason to test, monitor, and individualize care.The Future: Better Options Coming
New drugs are in development that target only the anxiety-related parts of the GABA system, not the memory and coordination areas. Early trials of α2/α3-selective agonists show they reduce anxiety just as well as benzodiazepines-but without memory loss or balance problems. Phase II results from early 2024 were promising. These aren’t available yet, but they’re proof that the goal isn’t just to quit benzodiazepines-it’s to replace them with something safer.What You Can Do Today
If you’re on benzodiazepines:- Don’t panic. You’re not alone, and help is available.
- Don’t stop suddenly. Talk to your doctor about a taper plan.
- Ask for a cognitive baseline test-MoCA or MMSE.
- Start tracking your memory and balance. Note any falls, near-falls, or moments of confusion.
- Look into support groups. Real stories from people who’ve been through it make a huge difference.
- Watch for subtle signs: repeating questions, missing appointments, stumbling on stairs.
- Encourage a conversation with the doctor-not to judge, but to protect.
- Help with the taper. A calm, supportive presence makes withdrawal less scary.
Can benzodiazepines cause permanent brain damage?
No, benzodiazepines don’t cause permanent structural brain damage like a stroke or trauma would. Brain scans of long-term users show no shrinkage or lesions. But they do cause lasting functional changes-how the brain processes information slows down. These changes can persist for months or even years after stopping, especially with long-term use. Recovery is possible, but it’s not instant.
Is it safe to take benzodiazepines for insomnia long-term?
No. While they help with sleep in the short term, tolerance builds quickly. After a few weeks, you need higher doses for the same effect. Long-term use worsens sleep quality, reduces deep sleep, and increases next-day drowsiness. Cognitive decline and fall risk also rise. For chronic insomnia, cognitive behavioral therapy for insomnia (CBT-I) is more effective and safer long-term.
How long does it take to recover mentally after quitting benzodiazepines?
Improvement starts within weeks for many-processing speed and attention often bounce back in 4-8 weeks. But full recovery of memory, focus, and mental clarity can take 6-12 months. Some people report continued small improvements up to two years after quitting. Patience and consistency are key. Tracking progress helps you see gains you might otherwise miss.
Why is diazepam preferred for tapering over other benzodiazepines?
Diazepam has a very long half-life-up to 100 hours. This means it stays in your system longer, leading to smoother, more gradual withdrawal. Short-acting drugs like alprazolam or lorazepam leave the body quickly, causing sharp drops in drug levels that trigger intense withdrawal symptoms. Switching to diazepam allows for smaller, more controlled dose reductions.
Are there natural alternatives to benzodiazepines for anxiety?
There are no natural supplements that work like benzodiazepines, but some can help manage anxiety. Regular exercise, mindfulness meditation, and CBT have strong evidence for reducing anxiety symptoms. Magnesium, L-theanine, and valerian root may offer mild calming effects, but they’re not substitutes for prescribed medication. Always talk to your doctor before making changes-especially if you’re tapering.
Can I taper off benzodiazepines on my own?
It’s not recommended. Withdrawal can be dangerous, with risks including seizures and severe psychiatric symptoms. A doctor can help you choose the right taper plan, switch to a safer medication like diazepam if needed, and monitor for complications. Support groups are helpful, but they’re not a substitute for medical supervision.
Write a comment
Your email address will not be published.




12 Comments
They’re not just drugs-they’re mind-wiping tools disguised as calm. The FDA? Complicit. The pharma giants? They’ve been funding “studies” since the ’70s to bury the truth. I’ve seen it: people on benzos become hollow shells, forgetting birthdays, losing jobs, walking into walls-and no one talks about the surveillance state using this to pacify the masses. It’s not an accident. It’s a system. And now they want you to “taper” like it’s yoga. Ha. Wake up.
You’re all missing the point. Benzodiazepines are merely symptoms of a deeper collapse-Western civilization’s surrender to chemical compliance. The hippocampus doesn’t just forget names-it forgets meaning. We’ve outsourced our neurology to corporations and now we’re surprised when our souls go numb? This isn’t pharmacology-it’s existential surrender wrapped in a prescription bottle. And you call this ‘tapering’? Pathetic. The real taper is from the illusion of control.
If you're on benzos and worried about memory or falls, talk to your doctor about a slow taper. The Ashton Protocol works. Track your symptoms. Use diazepam if possible. Support groups help. You’re not broken-you’re just medicated too long. Recovery is real, but it takes time. Be patient with yourself.
Anyone who takes benzos for more than 2 weeks is an idiot. I’ve seen so many people turn into zombies on these things. My uncle took alprazolam for 15 years and now he can’t remember his own grandkids. He thought he was fine until he fell and broke his hip. No one warned him. Doctors are lazy. They hand out pills like candy. You don’t need drugs for anxiety. Just go outside. Lift weights. Breathe. Simple stuff. Stop being weak.
Let’s talk about the GABAergic cascade. Benzodiazepines bind to α1, α2, α3, and α5 subunits of the GABA-A receptor. The α1 subunit mediates sedation, α2/α3 mediate anxiolysis, and α5 is the memory killer-hippocampal overload. That’s why diazepam’s long half-life reduces synaptic rebound. The Ashton Protocol exploits pharmacokinetic lag to avoid glutamate excitotoxicity during withdrawal. Most people don’t know this. They think it’s just ‘tapering.’ Nah. It’s neurochemical recalibration. Also, avoid SSRIs during taper-serotonin syndrome risk spikes.
OMG I JUST QUIT AFTER 8 YEARS!!! 🥹😭 I was crying every night, forgetting my kids' names, falling down the stairs 3x last month... but I switched to diazepam and went 2% every 3 weeks. Now I can read a whole book without rereading the same page 10 times!! I cried when I remembered how to play piano!! 🎹💖 Thank you to the BIC forum!! You saved me!! 🙏✨
I didn’t know benzos could do this. I thought they were just for short-term help. I’ve been on them for anxiety since college. Now I’m scared. But I’m going to talk to my doctor. Maybe I can try CBT instead. I just want to feel like myself again.
While the clinical evidence regarding cognitive decline and fall risk is robust, it is imperative that any intervention be undertaken within a framework of individualized care. Abrupt cessation is contraindicated, and medical supervision remains non-negotiable. The Ashton Protocol, while empirically supported, requires contextual adaptation based on comorbidities, age, and psychosocial support systems. Patient autonomy must be preserved, but not at the expense of safety.
Oh wow so now we’re supposed to believe the government and Big Pharma aren’t in on this? Come on. Benzos were pushed hard in the 80s and 90s because they kept people docile while the economy crumbled. You think your anxiety is real? Maybe it’s just the system screaming through your synapses. And now they want you to taper slowly so you don’t wake up and realize you’ve been asleep for 20 years. I stopped cold turkey in 2019. Seizures? Yeah. But I saw the truth. Better that than live as a zombie in a Walmart parking lot waiting for my next script.
As a Nigerian-American, I’ve seen this in my family. My aunt took lorazepam for 12 years-she’d forget where she put her food, then blame the dog. Then one day she fell and broke her pelvis. No one talked about it. We just said ‘she’s getting old.’ But it wasn’t age. It was the pills. Now my cousin is tapering with diazepam. We’re all learning. 🌍❤️
This isn’t about fear. It’s about responsibility. If you’re on benzos, you owe it to yourself to understand the cost. Cognitive decline isn’t inevitable-but it’s predictable. Track your MoCA scores. Use apps. Join a group. Ask your doctor for alternatives. You’re not weak for needing help. You’re strong for seeking a better path. Recovery isn’t linear, but it’s possible. And you’re not alone.
Interesting how everyone ignores the metaphysical layer. The benzodiazepine isn’t the problem-it’s the modern condition that necessitates it. We’ve turned the self into a machine that needs tuning. The brain isn’t broken; society is. Tapering is just a bandage on a systemic wound. True healing requires dismantling the structures that make us feel unsafe, unloved, and disconnected. Until then, we’ll keep swallowing pills and calling it progress.