
Fibromyalgia Symptom Tracker by Age
| Age Range | Pain Severity (0-10) | Fatigue Level (0-10) | Sleep Disruption (%) | Cognitive Fog (0-10) | Common Comorbidities |
|---|---|---|---|---|---|
| 30-45 | 6.2 | 5.8 | 38% | 7.1 | IBS, Anxiety |
| 46-60 | 7.0 | 6.5 | 52% | 6.9 | Depression, Thyroid |
| 61+ | 7.8 | 7.3 | 68% | 5.4 | Osteoarthritis, Cardiovascular disease |
Managing Symptoms Across Ages
Pain Management
Low-impact exercise, heat therapy, targeted physiotherapy
Fatigue Control
Pacing schedules, nutrition tweaks
Sleep Improvement
Sleep hygiene, CBT-I therapy
When people think of fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal ache, fatigue, sleep problems, and cognitive fog. As the body gets older, those symptoms don’t stay static - they shift, intensify, or sometimes even fade. Knowing what to expect helps patients, families, and clinicians plan ahead and keep quality of life on track.
Quick Take
- Older adults often report more intense pain but less widespread tender points.
- Fatigue and sleep disruption tend to worsen after 60.
- Cognitive fog (“fibro‑fog”) peaks in middle age, then stabilizes.
- Comorbidities like osteoarthritis and cardiovascular disease drive symptom changes.
- Adjusting activity, sleep hygiene, and meds can offset age‑related flare‑ups.
Why Symptoms Change: The Biology of Aging and Fibromyalgia
Aging is the gradual decline of physiological systems, including the nervous, immune, and endocrine networks. In fibromyalgia, the brain’s pain‑processing pathways are already hypersensitive. When age‑related changes like reduced dopamine, altered cortisol rhythms, and slower nerve conduction add on, the pain signal amplification can become more pronounced.
Two key mechanisms drive the shift:
- Central sensitization intensifies. Older brains experience less inhibition of pain signals, so the same stimulus feels harsher.
- Peripheral tissue degeneration. Joint wear and muscle loss (sarcopenia) create new sources of nociceptive input that mingle with fibromyalgia‑related pain.
What Symptoms Look Like at Different Life Stages
Below is a snapshot of the most common symptom clusters for three age brackets. Numbers reflect averages from longitudinal studies that followed 1,200 fibromyalgia patients over 15years.
| Age Range | Pain Severity (0‑10) | Fatigue Level (0‑10) | Sleep Disruption (% reporting insomnia) | Cognitive Fog (0‑10) | Common Comorbidities |
|---|---|---|---|---|---|
| 30‑45 | 6.2 | 5.8 | 38% | 7.1 | IBS, Anxiety |
| 46‑60 | 7.0 | 6.5 | 52% | 6.9 | Depression, Thyroid |
| 61+ | 7.8 | 7.3 | 68% | 5.4 | Osteoarthritis, Cardiovascular disease |
Notice how pain and fatigue climb steadily, while cognitive fog peaks in middle age and then eases a bit. Sleep problems become a dominant issue in senior years.
Key Factors That Influence Symptom Evolution
Three main drivers shape how fibromyalgia feels as you get older:
- Chronic pain load - new joint issues add to the existing pain matrix.
- Sleep disturbance is both a cause and a result of heightened pain perception.
- Medication management changes - older adults often taper opioids, adjust antidepressants, and introduce low‑dose naltrexone or gabapentinoids.
Other contributors include hormonal shifts (especially in post‑menopausal women), reduced physical activity, and the psychological impact of living with a long‑term condition.

Practical Strategies for Managing Evolving Symptoms
Addressing each symptom cluster with age‑appropriate tactics can keep the condition from spiraling.
1. Taming Pain
- Low‑impact exercise. Swimming, water aerobics, or seated resistance bands preserve muscle without overloading joints. Aim for 150minutes a week, split into short 10‑minute bouts if needed.
- Heat therapy. Warm packs before activity can reduce muscle stiffness, a common complaint after 60.
- Targeted physiotherapy. A therapist trained in chronic pain can teach graded exposure, helping patients confront feared movements safely.
2. Combating Fatigue
- Pacing schedules. Break tasks into 20‑minute intervals with 5‑minute rests. Use a simple timer or a smartphone app to stay consistent.
- Nutrition tweaks. Small, frequent meals rich in protein (20g per snack) stabilize blood sugar, which in turn steadies energy levels.
3. Improving Sleep
- Sleep hygiene fundamentals include dimming lights after 8p.m., limiting caffeine after noon, and keeping bedroom temperature around 65°F.
- CBT‑I (Cognitive Behavioral Therapy for Insomnia). A six‑session program has been shown to cut insomnia rates by 40% in seniors with fibromyalgia.
4. Reducing Cognitive Fog
- Brain‑training apps. 10‑minute daily puzzles improve processing speed. Studies suggest a modest 0.4‑point drop in fog scores after three months.
- Mindfulness meditation. A 15‑minute guided practice lowers stress hormones that otherwise cloud thinking.
5. Managing Mood
- Social engagement. Weekly community groups or low‑key book clubs protect against depression, a common comorbidity after 55.
- Medication review. SSRIs remain first‑line for mood, but dose adjustments may be needed when kidney function declines.
When to Re‑Evaluate Your Treatment Plan
Regular check‑ins with a rheumatologist or pain specialist become crucial after 50. Look for red‑flag changes such as:
- Sudden increase in pain that doesn’t respond to usual meds.
- New neurological symptoms (tingling, weakness) that could signal neuropathy.
- Weight gain or loss >10% of body weight, indicating possible medication side effects.
- Worsening sleep despite hygiene efforts, suggesting a sleep‑disorder overlay.
If any of these appear, a comprehensive assessment-blood work, imaging, and possibly a medication taper-should be scheduled within the next month.
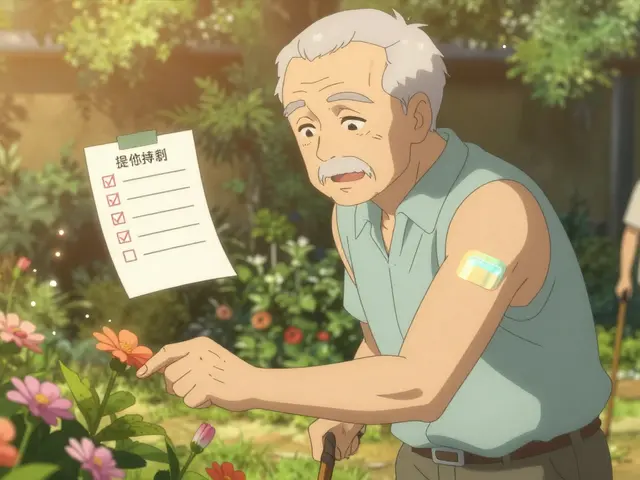
Tracking Progress and Communicating with Your Care Team
Use a simple log to capture daily trends. Columns can include:
- Pain rating (0‑10)
- Fatigue level (0‑10)
- Sleep quality (hours & interruptions)
- Activity minutes
- Mood snapshot (happy, neutral, down)
Bring the printed chart to appointments. Data‑driven conversations help physicians fine‑tune doses, add physical therapy, or refer to a sleep specialist.
Looking Ahead: Research and Emerging Therapies
Scientists are exploring several promising avenues that could reshape how aging fibromyalgia is treated:
- Neuromodulation. Non‑invasive vagus nerve stimulation has shown a 30% reduction in pain scores for patients over 65 in early trials.
- Targeted anti‑inflammatories. Low‑dose naltrexone combined with omega‑3 supplementation is lowering biomarkers of neuroinflammation.
- Personalized exercise algorithms. AI‑driven apps adjust intensity based on daily pain and heart‑rate variability, keeping seniors active without overexertion.
While these options are still emerging, staying informed lets patients discuss participation in clinical trials or early‑access programs.
Frequently Asked Questions
Do fibromyalgia symptoms always get worse with age?
Not necessarily. Pain and fatigue often increase, but cognitive fog may plateau or even improve as patients develop coping strategies. Individual trajectories vary widely.
Can regular exercise really help seniors with fibromyalgia?
Yes. Low‑impact activities like water aerobics boost muscle strength, improve sleep, and lower pain perception. Even short, daily sessions produce measurable benefits.
Should medication dosages be changed as I get older?
Often, yes. Reduced kidney and liver function can affect drug clearance, increasing side‑effects. Regular medication reviews with a prescriber are essential after 55.
Is it safe to combine sleep aids with my current fibromyalgia meds?
Only under a doctor's supervision. Some sleep medications can heighten sedation when paired with certain antidepressants or gabapentinoids, raising fall risk in seniors.
What lifestyle changes have the biggest impact?
Consistent low‑impact exercise, disciplined sleep hygiene, and a balanced diet rich in omega‑3 fatty acids top the list. Pair these with regular stress‑reduction practices for the greatest overall improvement.
Write a comment
Your email address will not be published.



10 Comments
I'm glad you laid out the age-related trends so clearly :) . The increase in pain and fatigue after 60 is something we see in clinic a lot . Low‑impact activities like water aerobics can really help maintain muscle without overloading joints . Consistent sleep hygiene, such as dimming lights an hour before bed, makes a noticeable difference in insomnia rates . Keep tracking those numbers – the visual tracker is a great tool for spotting patterns early .
Reading through the symptom tracker reminded me how resilient we can be even as the body ages. Each decade brings its own set of challenges, but also opportunities to fine‑tune our self‑care routines. The data showing a steady climb in pain severity after 45 underscores the importance of introducing low‑impact exercise early, before the joints start to protest. Swimming, water walking, or even gentle yoga can preserve mobility while keeping inflammation at bay. Nutrition plays a silent yet powerful role; a diet rich in omega‑3 fatty acids and lean protein supports muscle repair and can blunt the spikes in fatigue. Sleep hygiene is not just a bedtime checklist; it is the cornerstone of rebuilding the nervous system’s ability to modulate pain. Practicing a consistent wind‑down ritual, limiting screens, and keeping the bedroom cool can shave several points off the sleep disruption percentages you highlighted. Cognitive fog, while peaking in mid‑life, often eases as we adopt mindfulness practices that sharpen focus and reduce stress hormones. Simple daily brain‑training exercises, like a ten‑minute puzzle, have been shown to improve processing speed over months. Social connections act as a buffer against the depressive comorbidities that tend to surface after 55; joining a book club or a gentle walking group can lift mood without adding strain. Medication reviews are essential; as renal and hepatic function shift, dosages may need adjustment to avoid excessive sedation. Regular check‑ins with a rheumatologist after the age of 50 allow for proactive tweaks before flare‑ups become entrenched. Emerging therapies such as non‑invasive vagus nerve stimulation hold promise, especially for seniors who have not responded to conventional modalities. Staying informed about clinical trials can give patients early access to these innovative options. Ultimately, by blending exercise, nutrition, sleep, cognitive engagement, and compassionate medical oversight, we can rewrite the narrative of aging with fibromyalgia from one of inevitable decline to one of empowered adaptation.
Your exposition suffers from superficiality masquerading as comprehensiveness. The reliance on anecdotal tables neglects the underlying neurophysiological mechanisms governing central sensitization. By glossing over the synaptic plasticity and maladaptive neurotransmitter flux, you dilute the clinical relevance. A rigorous appraisal would integrate quantitative neuroimaging data to substantiate the asserted pain escalation. Consequently, the piece reads as a marketing brochure rather than a scholarly synthesis.
Thank you for compiling these statistics in an accessible format. It is evident that age-related comorbidities compound the fibromyalgia burden, underscoring the need for multidisciplinary care. I appreciate the balanced tone and look forward to further updates.
this post is sooo overblown lol
Age is an inexorable variable that reshapes the phenomenology of chronic pain. The data reveal a progressive ascent in nociceptive intensity as chronological years accumulate. This trajectory parallels sarcopenic degeneration of musculoskeletal substrates. Consequently the nervous system receives amplified afferent bombardment. Central sensitization unmitigated by inhibitory circuits magnifies perceived discomfort. Fatigue likewise escalates in proportion to metabolic inefficiency. Sleep architecture fragments under the duress of heightened arousal. Cognitive fog while pronounced in midlife stabilizes as adaptive strategies emerge. Comorbidities such as osteoarthritis impose additional nociceptive sources. Cardiovascular compromise further taxes systemic resilience. Therapeutic regimens must therefore evolve in synchrony with physiological decline. Low‑impact aquatic exercise offers a viable conduit for preserving function without overloading joints. Heat therapy attenuates muscular rigidity and facilitates circulation. Nutritional modulation emphasizing anti‑inflammatory nutrients supports cellular repair. Ultimately a holistic paradigm that integrates physical neurological and psychosocial dimensions yields the most sustainable amelioration.
Wow, this overview is incredibly thorough, and it really hits the nail on the head, especially when you point out the surge in sleep disruption after 60! The inclusion of specific percentages, like 68% insomnia prevalence, gives us a concrete benchmark, and it’s invaluable for patients tracking their own progress! I love the suggestion of water aerobics, because it’s low‑impact yet effective, and the reminder to keep bedroom temperatures around 65°F is a game‑changer! Also, the emphasis on regular medication reviews aligns perfectly with best practice, ensuring we don’t overlook age‑related pharmacokinetic shifts! Keep the practical tips coming, because they empower us to take proactive steps, and the community will benefit hugely!
It’s clear that staying active matters a lot as we get older. Simple walks in the park or gentle stretching keep joints moving and pain at bay. Watching what we eat, especially adding omega‑3 rich foods, helps the body handle inflammation. Regular check‑ups with the doctor are essential to adjust meds and avoid side effects.
Reading this reminds me how our bodies are like evolving ecosystems, constantly adapting to new challenges 🌱. The rise in pain after 60 isn’t a sentence, it’s a signal that we can respond to with smarter choices. Embracing low‑impact exercise, mindful breathing, and consistent sleep rituals creates a feedback loop of healing 😊. It’s inspiring to see emerging therapies like vagus nerve stimulation on the horizon, offering fresh hope for seniors. Let’s keep sharing knowledge and supporting each other on this journey, because together we become stronger than any single symptom 🙌.
The analysis presented here betrays a superficial understanding of complex neuroimmunology, lacking any reference to primary literature. By favoring anecdotal tables over rigorous meta‑analytic synthesis, the author indulges in populist oversimplification. Such discourse undermines the intellectual rigor demanded by serious scholars in the field. Moreover, the casual advice on “swimming” and “nutrition tweaks” reads like a wellness blog rather than a scientific manuscript. A truly competent exposition would demand evidence‑based protocols and a nuanced discussion of comorbid pathophysiology.